Medical credentialing is the process of checking a healthcare provider’s background. Their education, training, licenses, and work experience ensure they are qualified to care for patients safely. It helps keep healthcare trustworthy, safe, and compliant with laws and standards.
Credentialing isn’t just a formality. It protects patients, ensures providers meet legal requirements, and helps them get paid on time by insurance companies. Without proper credentialing, providers may face claim denials, payment delays, or legal problems.
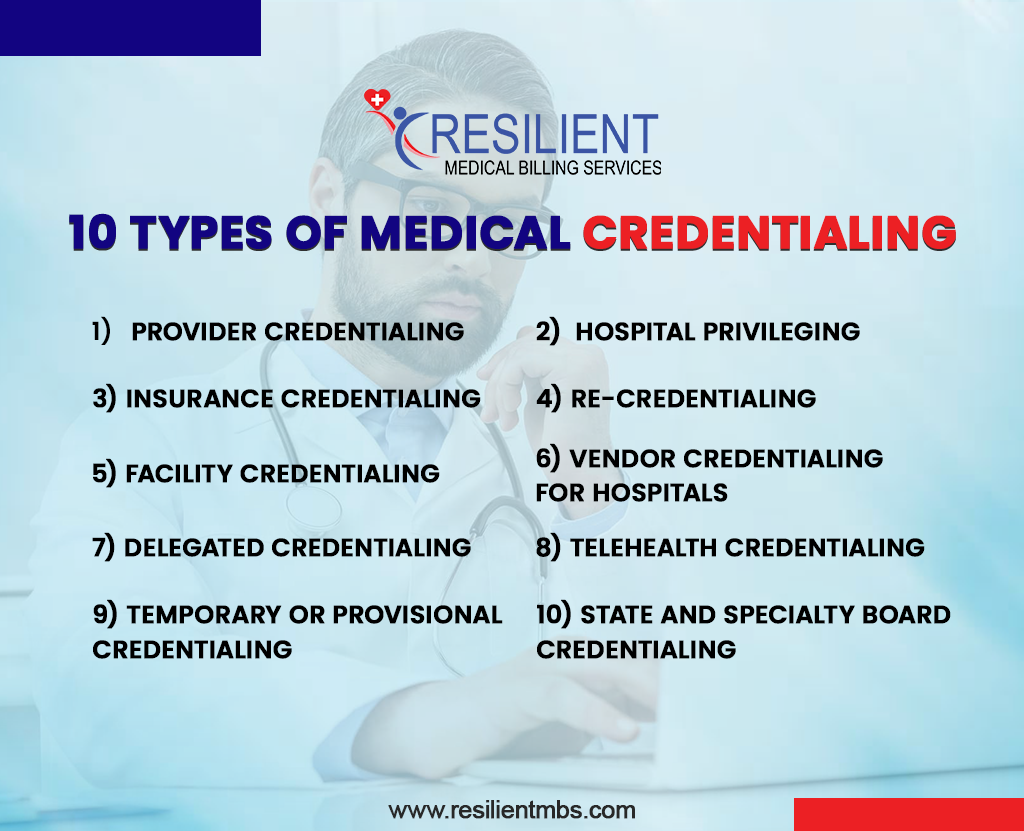
In this article, you’ll learn about the 10 main types of medical credentialing every healthcare provider should know. Understanding these can help you run your practice smoothly, earn patient trust, and avoid billing issues.
What is Medical Credentialing?
Medical credentialing is the formal process of verifying a healthcare professional’s qualifications, education, licenses, board certifications, training, malpractice history, and work experience to ensure they are qualified to deliver safe patient care.
Proper credentialing supports payer enrollment, hospital privileges, and compliance with regulatory and accreditation standards. Accurate credentialing reduces the risk of claim denials, protects patients, and speeds reimbursement.
Why Credentialing Matters (Compliance, Payment & Safety)
Proper credentialing affects three critical areas: patient safety, regulatory compliance, and revenue flow. Payers and hospitals require verified credentials before accepting claims or granting clinical privileges; gaps in credentialing can cause claim denials, delayed payments, inability to join provider networks, and liability exposures.
Understanding the types of credentialing in medical billing helps practices prioritize resources and avoid operational disruptions.
10 Types of Medical Credentialing
Below are the ten core types of medical credentialing every provider and practice manager should understand. Each entry includes what’s checked, typical documents, common timelines, and practical tips.
1. Provider Credentialing
What it is: Verifying an individual clinician’s license(s), education, board certification(s), DEA registration, malpractice claims history, and employment references so they may join payer networks.
Docs: Medical degree, state licenses, board certificates, CV, malpractice declarations, NPI.
Timeline: 45–120 days (varies by payer).
Tip: Keep a live CAQH/ProView profile and a credentialing binder with scanned docs to accelerate enrollment.
2. Hospital Privileging
What it is: Separate from credentialing, privileging grants permission to perform specific procedures at a hospital based on demonstrated competence. Hospitals review case logs, proctorship, and references.
Docs: Procedure logs, peer evaluations, and CME specific to privileges.
Tip: Prepare procedure-specific competency evidence before applying for OR privileges.
3. Insurance Credentialing
What it is: Enrollment and contracting with Medicare, Medicaid, and private payers to enable the provider to bill and be reimbursed. This step produces payer IDs and fee schedules.
Docs: CAQH attestation, W-9, EFT details, license, DEA, malpractice.
Timeline: 30–120 days; Medicare (PECOS) timelines vary.
Tip: Apply to Medicare via PECOS and maintain CAQH updates to avoid credential gaps.
4. Re-Credentialing
What it is: Periodic re-verification (commonly every 24–36 months) of all credentials and disciplinary history to maintain active status with payers and hospitals.
Docs: Updated licenses, malpractice renewals, and peer review summaries.
Tip: Automate re-credentialing reminders 6 months before expiry.
5. Facility Credentialing
What it is: Verifying the organizational licenses, accreditations (e.g., JCAHO), safety programs, and staffing standards for ambulatory surgery centers, clinics, and hospitals.
Docs: State facility license, accreditation certificates, policies (infection control, HIPAA), facility surveys.
Tip: Maintain an enterprise credentialing calendar for renewals.
6. Vendor Credentialing for Hospitals
What it is: Background checks, insurance verification, and safety training for external vendors, equipment reps, and contractors who need clinical-area access.
Docs: Proof of insurance, OSHA training, background checks.
Tip: Use a vendor portal to centralize credentials and automate renewals.
7. Delegated Credentialing
What it is: When payers delegate credentialing authority to a healthcare organization (e.g., a hospital or large group) under NCQA rules, the organization performs primary verification.
Docs & Controls: Local credentialing files plus audit evidence for delegate oversight.
Tip: Keep audit documentation and standardized processes to pass payer spot checks.
8. Telehealth Credentialing
What it is: Verification of licensure, telemedicine privileges, and technology/security compliance so providers can deliver care across state lines (where permitted).
Docs: Multi-state licenses or telemedicine registrations, HIPAA-compliance attestations.
Tip: Confirm state telehealth reciprocity and credentialing waivers during emergencies.
9. Temporary or Provisional Credentialing
What it is: Short-term approvals used in staffing shortages, emergencies, or locum tenens situations. Key documents are verified quickly, with formal credentialing completed later.
Docs: Primary source verification of state license and malpractice insurance; full file added later.
Tip: Use provisional credentialing only with clear time limits and supervised practice.
10. State and Specialty Board Credentialing
What it is: Ongoing maintenance of state medical board requirements and specialty board certifications (e.g., ABMS boards), including CME and MOC activities.
Docs: Board certificates, CME logs, license renewals.
Tip: Track state and specialty recertification windows in one dashboard.
Need help with provider credentialing or re-credentialing? Resilient MBS handles CAQH, PECOS, and payer enrollment for clinics and hospitals.
Common Credentialing Pitfalls and How to Avoid Them
- Outdated CAQH / PECOS info: Keep CAQH and PECOS profiles current; payers re-check these as first source documents.
- Incomplete primary-source verification: Ensure verification of primary sources for licenses and diplomas; payers will audit this.
- Gaps in malpractice or gap-in-care explanations: Always include signed explanations and supporting documents for any gaps >90 days.
- Failure to track expirations and renewals: Automate 180/90/30-day reminders for all critical credentials to prevent network deactivation.
When to Outsource Credentialing
Outsourcing is innovative when internal bandwidth is limited, when a practice operates across states, or when rapid payer enrollment is required. A professional credentialing partner (like Resilient MBS) typically provides: CAQH and PECOS management, payer follow-up, primary source verification, re-credentialing tracking, and audit-ready documentation.
Expect clear SLAs (turnaround times), an onboarding checklist, and monthly status reporting. Outsourcing ROI is usually seen as fewer enrollment delays, reduced claim denials, and faster revenue realization.
Wrap-Up
Understanding these types of medical credentialing helps organizations prioritize work, avoid payer enrollment pitfalls, and maintain continuous revenue flow. Start by auditing your current credentialing gaps, centralizing documents, and creating renewal reminders.
If this process is overwhelming, Resilient MBS offers complete credentialing services for providers and facilities, from CAQH setup to ongoing re-credentialing support.
FAQs
What are the most common credentialing types for doctors?
Most common types include provider credentialing, payer credentialing, hospital privileging, re-credentialing, and state/specialty board credentialing.
How long does provider credentialing take?
Typical timelines range from 45–120 days for payer enrollment; Medicare (PECOS) and some state programs vary.
What documents do I need for medical credentialing?
Key documents: medical degree, active state license, board certification (if applicable), DEA certificate, malpractice insurance declarations, CV, primary source verifications, and NPI.
What is delegated credentialing, and is it safe?
Delegated credentialing allows an organization to perform credentialing under payer oversight. It’s efficient and safe when the organization uses NCQA-compliant processes and records audit trails.
Can credentialing issues cause claim denials?
Yes, incomplete or expired credentialing can lead to payer rejections, network deactivation, and subsequent claim denials or payment delays.










