Medical billing is the backbone of the revenue cycle when it comes to getting paid in healthcare. At the heart of every successful claim lies accurate coding—and a crucial but often overlooked part of this process is the Entity Code in Medical Billing.
One piece of this puzzle that often flies under the radar is entity codes. These identifiers play a vital role in the claim process by telling insurers exactly who is involved, whether it’s a provider, a facility, or an organization. They guide claims through the right channels for approval and payment.
But when entity codes are incorrect or missing, problems follow. Think claim rejections, delayed payments, or even outright denials. This is why it is important for administrative teams, billing professionals, and healthcare providers to not only comprehend entity codes, but also to employ them accurately consistently.
What is an Entity Code in Medical Billing?
An entity code in medical billing refers to a specific identifier used to classify the party involved in a healthcare transaction. This party could be an individual healthcare provider, a healthcare organization, or a billing service.
The entity code meaning in medical billing extends beyond just identification. It ensures claim attribution and processing according to payer and system rules.
What Is an Entity ID number?
An entity ID number is a unique identifier used within electronic transactions, often in conjunction with standards set by the Health Insurance Portability and Accountability Act (HIPAA). This number helps distinguish between multiple entities that may be involved in the billing and claims process.
What is an Entity code in Medical Billing exactly?
It is a code that identifies applicants and their roles. It is essential during claim adjudication and ensures all parties are represented.
Clearinghouses and payers may reject applications with incorrect entity codes, requiring rework and resubmission. Understanding entity ID numbers and how they work in medical billing is important for any healthcare institution looking to simplify its revenue cycle.
Common Places You’ll See an Entity Code on Claim
In healthcare claims processing, entity codes are vital for identifying the roles of individuals or organizations involved in a claim. Found on both CMS-1500 and UB-04 forms, these standardized identifiers help ensure accurate adjudication.
On the CMS-1500, entity codes appear in sections like Box 24J to indicate whether a provider is an individual or an organization. On the UB-04, they identify billing providers, payers, and service facility locations.
By defining roles such as provider, patient, payer, or referring provider, entity codes streamline claim interpretation, validate participant relationships, and support efficient processing through clearinghouses and payer systems.
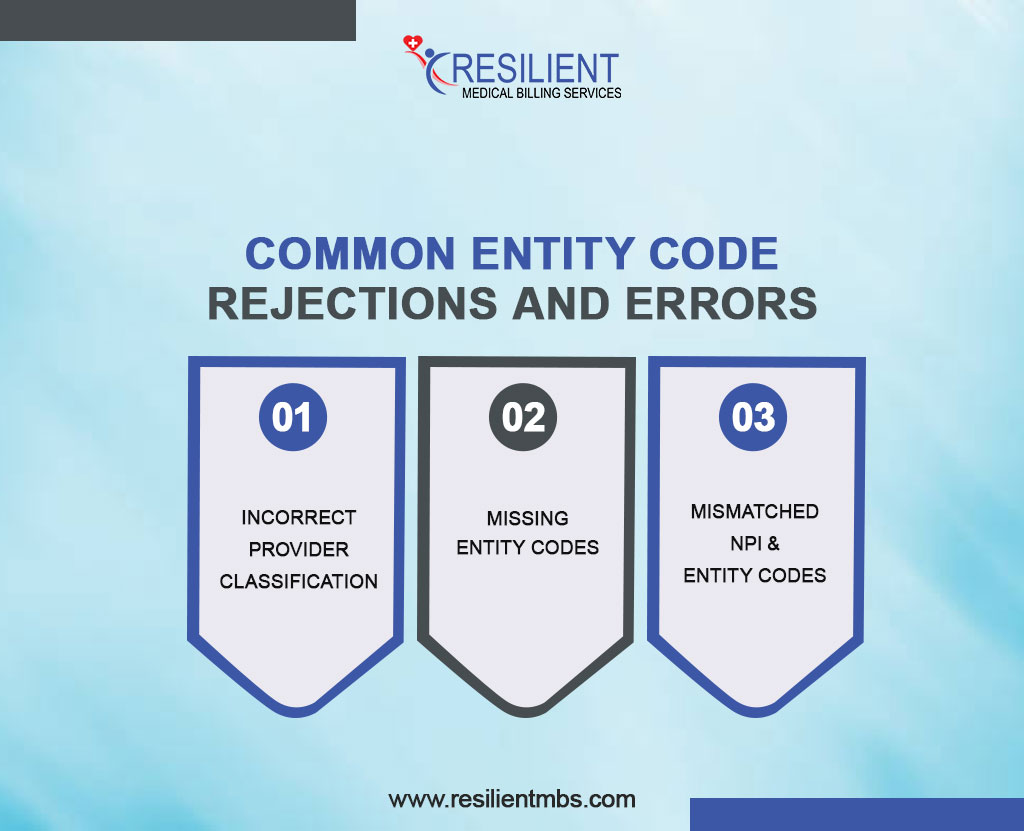
Common Entity Code Rejections and Errors
Despite their standardized nature, entity codes can sometimes lead to claim rejections when used incorrectly. Entity code rejection is a common obstacle that providers and billers encounter during the electronic data interchange (EDI) process.
These rejections typically arise due to mismatched, missing, or inappropriate use of entity codes on claim submissions.
Some of the most frequent causes of entity code rejection include:
- Incorrect provider classification: Using an entity code that designates an individual instead of an organization when billing under a group practice.
- Missing entity codes: A required code may be left blank, especially in fields designating the referring provider or service facility.
- Mismatched NPI and entity codes: The National Provider Identifier (NPI) must align with the entity code; otherwise, the claim can be rejected for identity inconsistency.
Entity Code List for Medical Billing
Entity codes are essential in medical billing because they identify each party in a healthcare transaction. Each provider, patient, payer, and referring physician has an entity code to ensure accurate communication and claim processing between healthcare providers and insurance companies.
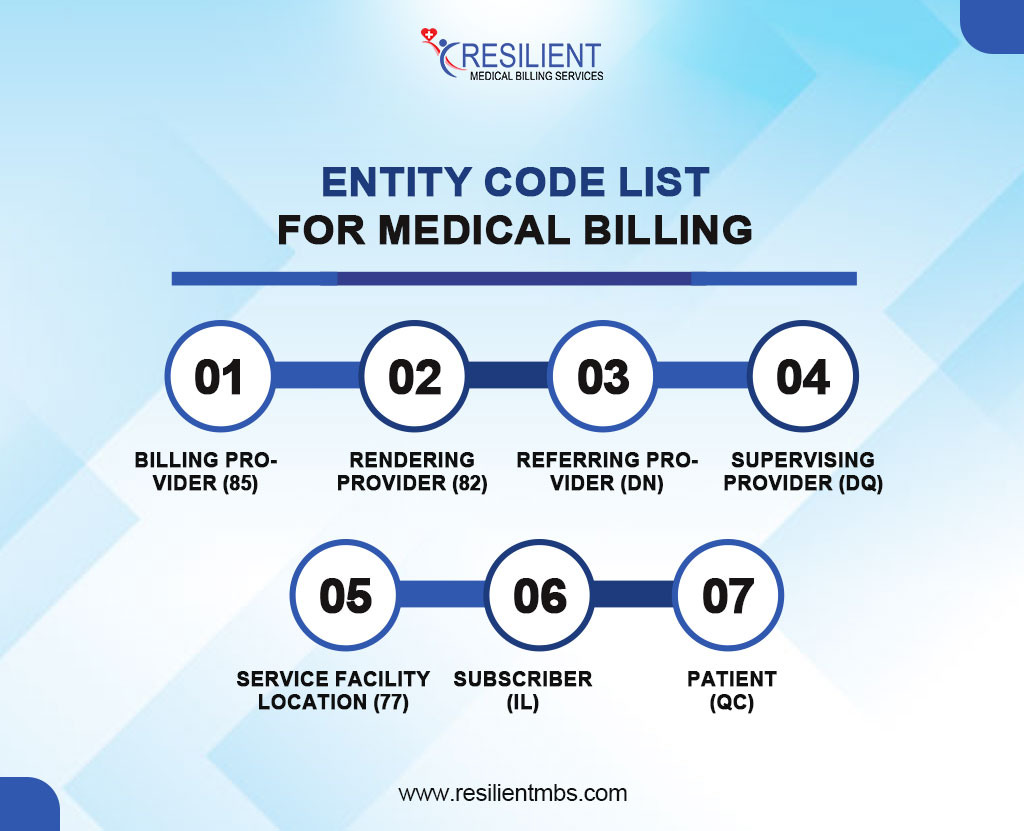
A general entity code list medical billing typically includes identifiers such as:
Billing Provider (85): Refers to the individual or organization submitting the claim.
Rendering Provider (82): The provider who performed the service.
Referring Provider (DN): The physician who referred the patient for services.
Supervising Provider (DQ): A provider overseeing the services rendered.
Service Facility Location (77): The physical location where the services were provided.
Subscriber (IL): The individual carrying the insurance policy.
Patient (QC): The recipient of medical services.
Who Governs or Assigns Entity Codes?
Entity codes are standardized through collaboration among key organizations rather than a single authority. HIPAA mandates the use of standardized electronic transactions, supported by ASC X12N, which develops EDI formats like the 837 form that includes entity code specifications.
CMS further shapes how these codes are applied, setting guidelines often followed by other payers. While there’s no central registry for all entity codes, the widespread adoption of X12 standards under HIPAA has led to broad consistency across systems.
Though minor variations exist, billing professionals can rely on EDI guidelines and payer documentation for accurate use. Ongoing training and updates from vendors and clearinghouses support continued compliance.
Final Thoughts!
Understanding medical billing entity codes improves your revenue cycle, not simply claims processing. These codes define healthcare transaction responsibilities, ensuring claims are accurately interpreted and reimbursed.
Entity code errors can cause costly delays and rejections, but they can be avoided with the correct knowledge and systems. Staying educated and watchful helps boost claim acceptance and revenue cycle efficiency.
Need help ensuring accurate billing and claim submission?
Contact Resilient MBS LLC today for expert support in medical billing, coding, and claim resolution. We help providers eliminate coding confusion—so you can focus on patient care.