Ever received a claim denial and wondered what went wrong? Denial codes are the key to unlocking that answer. These standardized codes are based on the Claim Adjustment Reason Codes (CARC) system, explaining why a claim wasn’t reimbursed and how you can fix it.
One important code to understand is Denial Code PR 272, which can directly impact your revenue flow if not handled properly. In this blog, we’ll break down what PR 272 means, why it happens, and the steps you can take to resolve it efficiently.
Whether you’re a billing specialist or a practice administrator, this guide will help you submit cleaner claims and get paid faster.
What is Denial Code PR 272?
Denial Code PR 272 is issued when a claim is denied because the patient did not respond to the insurer’s request for additional information. It means the insurer cannot verify eligibility or benefits without the required details.
The “PR” prefix indicates the denial is due to patient responsibility, not a provider or payer error.
Relevance in Payer Communications
PR 272 commonly appears in communications from insurers like Blue Cross Blue Shield (BCBS) when patient input is needed, such as coordination of benefits (COB) forms, accident reports, or third-party liability details. If the patient does not respond, the claim remains unprocessed.
Distinction from Similar Denial Codes
It is important to distinguish PR 272 from other codes, such as:
PR-27 Denial code Description –This code indicates that the patient is not eligible for services on the date of service.
CO 272 – Uses the same code number (272) but with the “CO” prefix, signifying that the provider is responsible for the denial due to missing information.
Understanding these differences helps physicians read denials and take the necessary actions, which are contacting the patient, appealing the claim, or amending documents.
CO 272 Denial Code Resolution Steps
- Review Insurance Contract Terms
Confirm if the service is explicitly excluded or not covered under the patient’s plan.
- Verify Patient Eligibility and Coverage
Double-check the patient’s eligibility for the date of service, plan benefits, and exclusions using the payer portal.
- Check Coding and Billing Accuracy
Ensure that the correct CPT/HCPCS codes and modifiers were used and that they align with covered services.
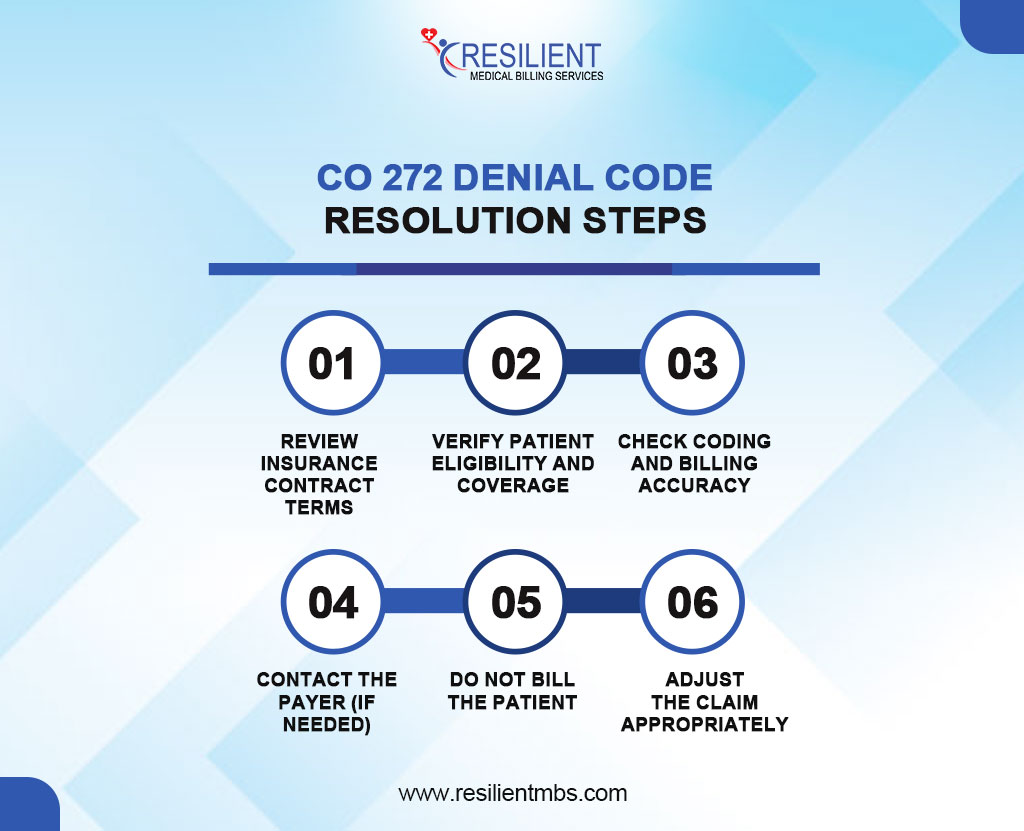
- Contact the Payer (If Needed)
If coverage seems likely, but the service was denied, contact the payer to clarify the denial reason.
- Do Not Bill the Patient
Since this is a contractual obligation (CO) denial, the denied amount cannot be transferred to the patient.
- Adjust the Claim Appropriately
Write off the denied amount per your contractual agreement with the payer and document the adjustment.
Common Reasons for Denial Code PR 272
- Eligibility Issues
The patient’s coverage may have lapsed, been terminated, or not been active on the date of service.
- Non-Covered Services
The procedure may fall outside the patient’s plan, such as elective, experimental, or non-medically necessary treatments.
- Incomplete Insurance Verification
Failure to confirm coverage details, effective dates, or authorization requirements can result in rendering non-covered services.
- Plan Exclusions or Limitations
Services exceeding visit caps, performed by out-of-network providers, or restricted under the plan are common denial triggers.
How PR 272 Can Appear in Different Formats
Denial codes may vary by payer. PR 272 typically indicates patient responsibility, but some systems may show it as CO 272, meaning a contractual denial with no patient responsibility. Accurate interpretation is key for proper follow-up.
PR 272 vs. PR 27 Denial Codes
- PR 272 denial code BCBS means the patient is eligible, but the service isn’t covered.
- PR 27 denial code reason means the patient isn’t eligible for coverage on the date of service.
Understanding the difference helps ensure proper appeal handling and prevents workflow errors.
How to Resolve Denial Code PR 272 – Solutions For PR 272 Denial Code
Resolving a denial under PR 272 requires a thorough and structured approach to determine the root cause and take corrective actions.
Below is a step-by-step guide for effective resolution:
- Verify Patient’s Insurance Coverage and Benefits
Review the patient’s plan to ensure the service is covered, including effective dates, limits, and exclusions.
- Contact the Payer for Clarification
Call the insurance company to confirm coverage details and whether additional documentation is needed.
- Educate Patients on Their Benefits Before Service
Inform patients about their coverage and limitations to help prevent future denials.
- Appeal if Services Were Wrongly Denied
Submit a detailed appeal with medical necessity documentation and supporting codes.
- Documentation and Communication Best Practices
Maintain clear records of all verifications and payer interactions, including dates and representative names.
How to Prevent Future PR 272 Denials
Minimize PR 272 denials with these proactive strategies:
- Verify Insurance Eligibility
Confirm patient coverage before each visit using payer portals or electronic tools. Check for service-specific limitations.
- Pre-Authorization & Benefit Checks
Secure required authorizations and confirm benefits for complex or costly services. Record auth numbers and expiration dates.
- Staff Training & Claim Audits
Train staff on denial causes and insurance verification. Conduct regular audits to spot and correct recurring issues.
- Utilize Practice Management Software
Use systems with real-time eligibility checks and denial alerts to flag uncovered services or discrepancies early.
Concluding Thoughts
Denial Code PR 272 reflects a service not covered under the patient’s benefit plan, typically due to eligibility issues or coverage limits. Preventing these denials starts with accurate eligibility checks, benefit verification, and proper documentation.
Managing PR 272 denials requires precision, expertise, and a proactive billing approach. If your practice faces recurring denials or insurance challenges, professional help can make a big impact.
Contact Resilient MBS to reduce denials, improve reimbursements, and strengthen your revenue cycle. Our experts identify the root causes and deliver customized solutions to protect your bottom line.