Fast. Simple. Secure. In-Network.
We unlock in-network access — even with the toughest payor panels.
We secure your spot in-network — no matter how selective the payors are.



Schedule a Call with Credentialing Expert
Let’s start with a few details about you and your organization.
- Ensuring enrollment in 30-90 Business day
- Bi-Weekly reports
- dedicated Credentialing Manager
- Aggressive follow-up
Credentialing, Done Right, Fast, Accurate, Reliable
Join thousands of providers who trust our medical credentialing solutions and proven process to streamline credentialing and maximize revenue, without the stress.
Credentialing, Done Right, Fast, Accurate, Reliable
Join thousands of providers who trust our medical credentialing solutions and proven process to streamline credentialing and maximize revenue, without the stress.
Resilient MBS Expedites the Payer Enrollment Process For Every Healthcare Entity
Credentialing is a vital step for healthcare providers to ensure compliance, build patient trust, and deliver quality care. Our end-to-end credentialing solutions support providers across all specialties, making the process seamless and stress-free. We offer credentialing services for:
Resilient MBS Expedites the Payer Enrollment Process For Every Healthcare Entity
Credentialing is a vital step for healthcare providers to ensure compliance, build patient trust, and deliver quality care. Our end-to-end credentialing solutions support providers across all specialties, making the process seamless and stress-free. We offer credentialing services for:
Expert Credentialing Services Customized to Your Practice

Hassle‑Free Payer Enrollment
Resilient MBS gathers your payer enrollment requirements, submits applications accurately, and manages follow‑up communications. You receive transparent status updates, prompt issue resolution, and faster approval timelines. Enjoy a seamless process that speeds reimbursements and frees your team to focus on patient care.

Stress‑Free Re‑Enrollment
Resilient MBS tracks your credential expiration dates, prepares renewal documents, and submits re‑enrollments on schedule. You get proactive reminders, real‑time status alerts, and dedicated support that prevents lapses. Maintain uninterrupted payer access and keep your practice compliant without added administrative strain
CAQH Profile
Management
Resilient MBS maintains your CAQH profile by updating licenses, malpractice coverage, and attestations. We handle verifications, run compliance checks, and send timely alerts. Keep your information current, accurate, and audit‑ready, without extra work.
Efficient ERA/EFT
Integration
Resilient MBS sets up ERA and EFT for commercial and government payers. We configure electronic remittance, verify connectivity, and resolve issues quickly. Enjoy faster payments, clear remittance details, and reliable fund transfers, no manual follow‑up needed.
Comprehensive License and Certification Management
Resilient MBS manages licenses and certifications for your providers, from applications to renewals across state boards. We monitor deadlines, coordinate submissions, and provide status updates. Count on expert guidance and compliance tracking that safeguards your credentials and reduces audit risk for your practice.
Expert Credentialing Services Customized to Your Practice

Hassle‑Free Payer Enrollment
Resilient MBS gathers your payer enrollment requirements, submits applications accurately, and manages follow‑up communications. You receive transparent status updates, prompt issue resolution, and faster approval timelines. Enjoy a seamless process that speeds reimbursements and frees your team to focus on patient care.

Stress‑Free Re‑Enrollment
Resilient MBS tracks your credential expiration dates, prepares renewal documents, and submits re‑enrollments on schedule. You get proactive reminders, real‑time status alerts, and dedicated support that prevents lapses. Maintain uninterrupted payer access and keep your practice compliant without added administrative strain
Optimized 7-Step Credentialing Journey for Healthcare Providers
1. Application Submission
Providers submit their personal, educational, & professional information.
2. Document Collection
Gather licenses, certifications, CV, references, malpractice insurance, & other relevant documents.
3. Primary Source Verification
HMS USA verifies credentials directly with issuing authorities.
4. Approval & Enrollment
Providers are approved to join insurance networks and practice.
5. Committee Review
Credentials are assessed by a credentialing committee for approval.
6. Background Checks
Criminal, malpractice, disciplinary, and federal sanctions are reviewed.
7. Ongoing Monitoring
Licenses, CME, and compliance are continuously tracked.

Experience Pure Satisfaction 100% Providers Customer Happiness with Rate 5-Star Reviews
At Resilient MBS Assist, we’re committed to delivering complete customer satisfaction through our trusted network of 5-star providers. Our innovative platform connects you with top-rated professionals and real reviews, so you can choose excellence every with confidence and experience service step of the way.
Key Benefits of Resilient MBS Credentialing Services
- One expert team handles rules for all states
- Simple intake process with minimal repeat paperwork
- Early detail checks prevent delays or rejections
- A single provider profile works across multiple plans
- IDs and records remain synchronized across systems
- Smooth enrollment from initial form submission to approval
- Facility privileges arranged on time
- Recredentialing tracked and filed before deadlines
- Contracts reviewed for fairness and clarity
- Short-term coverage set up to prevent billing gaps
- Transparent status updates with a dedicated contact
Make the switch to Resilient MBS 🡪

Explore Flexible Pricing Options
- Join with Zero Cost
- Act Before Time Runs Out
- Transparent Pricing
- Effortless credentialing just for you
- Special Discount For Groups
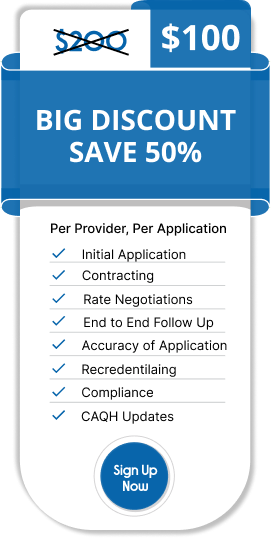
Put 10 + application and get Additional 10% discount
We Partner with Leading Insurance Providers














Accepted Insurances














Medical Credentialing Services FAQs
Medical credentialing is the process of verifying a healthcare provider’s qualifications, licenses, certifications, and professional background to enroll them with insurance payors and healthcare networks.
Credentialing ensures providers can participate in insurance networks, receive reimbursements, maintain compliance, and build trust with patients and payors.
The process typically takes 60-90 days, depending on the payor, provider type, and completeness of documentation. Some payors may take longer for exclusive panels.
Common documents include:
-State medical license
-DEA registration (if applicable)
-Board certifications
-CV/resume
-Malpractice insurance proof
-Work history
-References
Yes, our service manages credentialing for all major commercial, government, and private payors, including exclusive panels that are often hard to access.
CAQH (Council for Affordable Quality Healthcare) is a centralized database that stores provider information to simplify credentialing with multiple insurance plans. Completing CAQH profiles is often mandatory.
-Faster enrollment with payors
-Reduced administrative burden
-Accurate and complete documentation
-Minimized claim denials due to credentialing errors
-Dedicated follow-up on approvals
Yes, we handle both initial credentialing and re-credentialing, ensuring providers remain in-network without interruption.
Our team proactively tracks applications, communicates with payors, and resolves issues to ensure approvals are completed efficiently.
No, we handle credentialing for physicians, advanced practice providers (NPs, PAs), therapists, and other healthcare professionals who need in-network status.
Costs vary based on provider type and number of payors. Outsourcing is typically more cost-effective than managing credentialing in-house due to reduced staff time and faster enrollment.
Yes, we use expert tracking, CAQH optimization, and proactive payor communication to expedite approvals wherever possible.
We specialize in difficult and exclusive payor panels, provide real-time status updates, and ensure 100% compliance with payor and regulatory requirements.
Real Results from Real Providers
Case Study: We enroll clinical providers into premium payer networks in record time!
- Problem: Providers faced long delays in payer enrollment, leading to 4+ months of lost reimbursements and patient scheduling bottlenecks. The absence of streamlined credentialing caused gaps in network participation and significant revenue leakage.
- Solution: Implemented a dedicated credentialing team with automated CAQH updates, payer follow-ups, and compliance tracking. Customized workflow reduced administrative burden and ensured faster enrollment across major payers.
- Result: Result: Average credentialing time reduced by 50%, providers became billable in weeks instead of months, and the practice unlocked thousands in previously delayed reimbursements.
Ready to be enrolled?
Get a FREE consultation Now
















