As home healthcare grows, providers face increasing claim denials that delay payments and disrupt revenue flow. With more patients choosing care at home, especially older adults and individuals with chronic conditions, understanding and addressing home health claim issues has become vital.
This article highlights the main causes of home healthcare claim denials and offers proven strategies to prevent them.
Boost your revenue and reduce denials with Resilient MBS. Our experts streamline home healthcare billing, improve accuracy, and secure faster reimbursements.
Understanding Home Health Claims
A home health claim is submitted to insurance payers (like Medicare, Medicaid, or private insurers) to receive payment for at-home care services. Unlike standard medical claims, these often include multiple visits, extended care plans, and detailed documentation proving medical necessity.
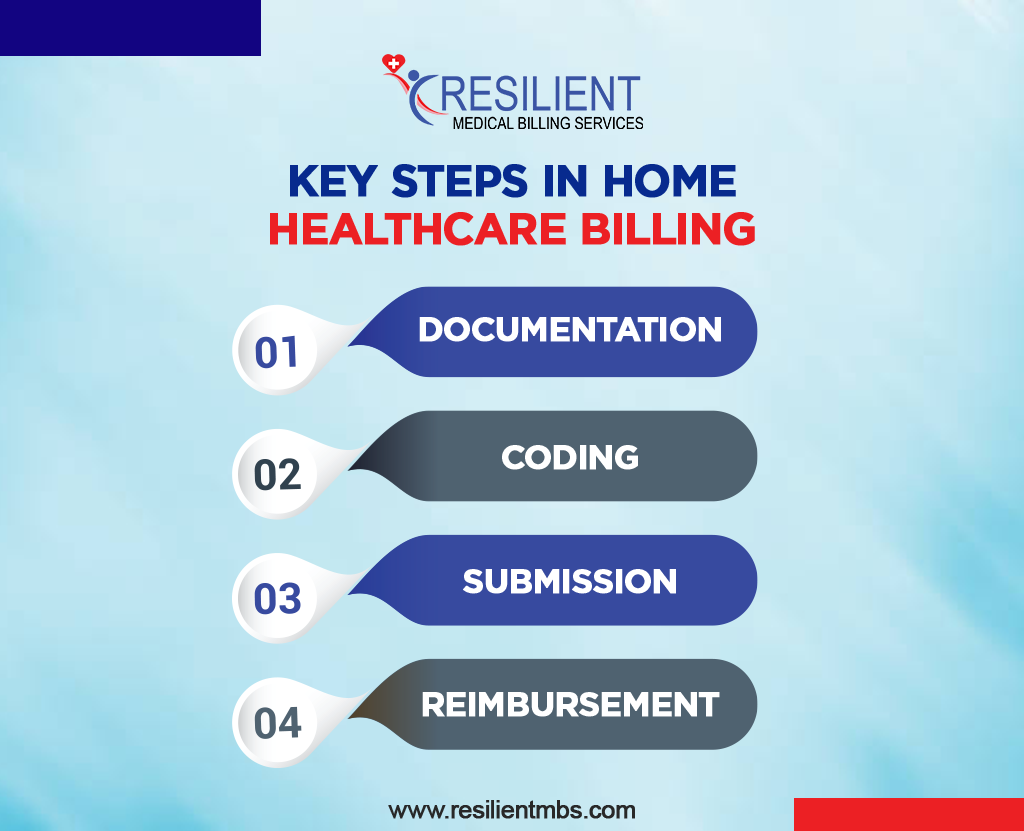
Key Steps in Home Healthcare Billing:
- Documentation: Complete patient records and signed physician orders.
- Coding: Accurate ICD-10, CPT, and HCPCS code selection.
- Submission: Sending the claim for payer review.
- Reimbursement: Payment issued upon approval.
Even small errors, like missing notes or incorrect insurance details, can trigger health insurance claim denials. Maintaining accurate documentation and compliance ensures smooth reimbursements and a steady cash flow.
Common Reasons for Home Health Claim Denials
Understanding the root causes of denials in medical billing helps providers take proactive steps to avoid revenue loss.
1. Incomplete or Inaccurate Documentation
Missing visit notes, physician signatures, or proof of medical necessity often cause denials. Ensure every patient record clearly supports the provided care.
2. Incorrect or Missing Codes
Coding errors (in ICD-10, CPT, or HCPCS) are a leading cause of denials. Regular code audits and staff training prevent costly mistakes.
3. Eligibility or Authorization Issues
Claims are rejected when insurance coverage isn’t verified or prior authorization is missing. Always confirm patient eligibility before services begin.
4. Late or Duplicate Submissions
Each payer has strict submission deadlines. Late or duplicate claims lead to automatic denials. Use tracking software to avoid delays.
5. Missing Itemized Statement in Medical Billing
An itemized statement in medical billing lists all services and costs. Without it, payers may question accuracy. Providing detailed statements speeds up approvals.
6. Non-Covered or Unverified Services
Services not covered by payer contracts or lacking verification result in denials. Review policies and documentation before submission.
The Financial and Operational Impact of Claim Denials
Frequent home health claim denials affect both financial stability and workflow. Each denied claim costs time and money, often an average of $25 to rework.
For small agencies, repeated denials disrupt operations, delay staff payments, and strain resources. Over time, poor denial management weakens payer relationships and lowers revenue predictability.
By addressing documentation gaps and verification errors early, providers can strengthen their revenue cycle management (RCM) and maintain consistent cash flow.
How to Solve and Prevent Home Health Claim Denials
Proactive denial management is key to maintaining a healthy billing cycle. Here’s how to minimize errors:
Use a Denial Tracking System
Monitor all denials and identify recurring issues, such as coding errors or missing documentation, to prevent future rejections.
Conduct Regular Audits
Review claims before submission to ensure accuracy and compliance with payer rules.
Verify Insurance Before Each Visit
Confirm patient eligibility and pre-authorization requirements before starting care.
Provide Itemized Billing
Offer a detailed itemized statement in medical billing to enhance transparency and trust with payers.
Train Your Billing Team
Educate staff on evolving payer rules, code updates, and documentation standards to ensure first-pass claim acceptance.
Leverage Automation and Professional Billing Support
Partnering with expert home healthcare billing companies like Resilient MBS can reduce administrative load, increase claim accuracy, and prevent denials before they occur.
Partner with Resilient MBS to eliminate denials, boost cash flow, and simplify your home healthcare billing process. Get your free billing audit today and see how our experts can help maximize your revenue.
Role of Technology and Outsourcing in Denial Prevention
Technology has transformed how providers handle denials in medical billing. Automation tools, including AI and RPA, can review claims, detect missing data, and reduce human error.
By outsourcing to professional home healthcare billing companies, providers benefit from:
- Accurate coding and claim submission
- Faster denial resolution and appeal processing
- Compliance with current payer and CMS regulations
- Improved efficiency and reduced overhead costs
Together, automation and expert support build a stronger, denial-free billing system.
Key Metrics to Monitor for Denial Reduction
Tracking performance helps agencies identify weaknesses and maintain efficiency.
- Claim Denial Rate: Lower rates mean better billing accuracy.
- Clean Claim Rate: High rates reflect correct documentation and code use.
- Average Days in A/R: Shorter turnaround equals faster reimbursements.
- Rework Percentage: Fewer resubmissions reduce administrative costs.
Consistent tracking of these metrics enables smarter decision-making and ongoing revenue improvement.
Common Mistakes to Avoid in Home Health Billing
Even minor mistakes can cause major disruptions in home healthcare billing. Avoid these pitfalls:
- Submitting incomplete or inaccurate claims
- Ignoring payer denial feedback
- Failing to follow up on unpaid claims
- Using outdated billing software or code sets
Regular process reviews, staff training, and software updates ensure compliance and accuracy.
Closing Words
Reducing home health claim denials is essential for maintaining financial health and providing quality patient care. Focus on documentation accuracy, timely follow-ups, and proper staff training to achieve consistent reimbursements.
FAQs
What causes most home health claim denials?
Missing documentation, incorrect codes, or eligibility issues are the leading causes of denials.
How can I prevent claim denials in home healthcare billing?
Verify insurance early, use correct codes, and ensure complete documentation before submission.
Why is an itemized statement important in billing?
It clarifies charges, prevents disputes, and supports claim transparency.
How do billing companies help improve reimbursements?
They handle coding, submission, and follow-ups, ensuring cleaner claims and faster payments.
Why is accurate documentation important?
It proves medical necessity, prevents health insurance claim denials, and supports compliance.










