Medical billing denials are a common challenge for healthcare providers. When a claim is denied, it can cause delays in payment, extra paperwork, and even lost revenue. Among the most common and frustrating issues faced by healthcare providers is the CO-252 Denial Code.
This denial code signals that a claim cannot be processed because key patient or claim-related information is missing or inaccurate. While it might sound minor, repeated CO-252 denials can disrupt your revenue cycle, delay reimbursements, and increase administrative workload.
At Resilient MBS, we specialize in helping healthcare organizations prevent and resolve denials like CO-252 efficiently, ensuring compliance, accuracy, and faster payments. Let’s explore what the CO-252 denial means, its root causes, and the best ways to resolve and prevent it.
Understanding the CO-252 Denial Code
CO-252 Denial Code Description
The CO-252 Denial Code indicates that a medical claim has been returned due to missing or incorrect patient responsibility or financial information. Essentially, the payer cannot process the claim until specific details are corrected.
This code acts as a reminder for billing teams that the claim is incomplete, not necessarily rejected, but paused until the required information is submitted correctly.
In simple terms, CO-252 means your claim needs corrections before the insurance company can pay.
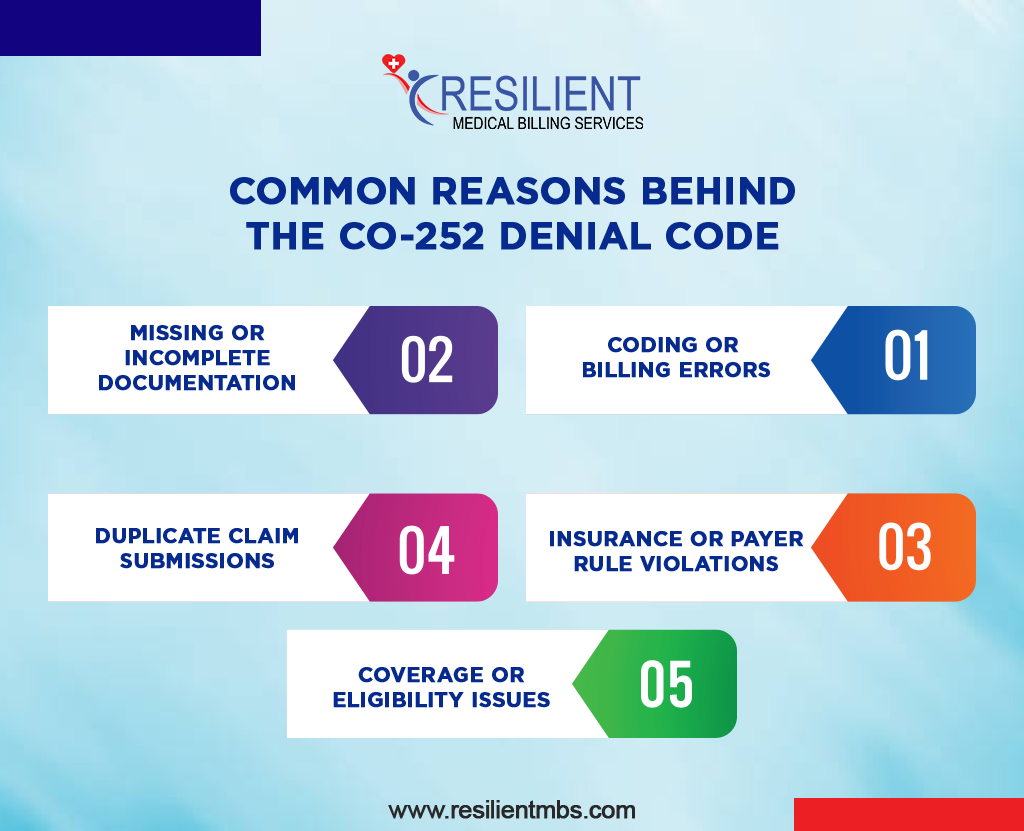
Common Reasons Behind the CO-252 Denial Code
Understanding the root causes of CO-252 denials helps prevent them from recurring. Here are the most common reasons:
1. Coding or Billing Errors
Incorrect CPT, HCPCS, or ICD-10 codes are among the top causes of CO-252 denials. These mistakes can occur when procedure codes don’t align with the documented services or diagnosis.
Example: Using an outdated procedure code or a mismatched diagnosis code that doesn’t support the service billed.
2. Missing or Incomplete Documentation
Claims often get denied when essential documentation, such as physician notes, authorizations, or consent forms, is missing.
Example: Failing to attach prior authorization for a diagnostic procedure or incomplete encounter notes.
3. Insurance or Payer Rule Violations
Each payer has unique billing and documentation requirements. Failing to follow these rules, such as omitting a required modifier or billing beyond the coverage limit, often triggers a CO-252 denial.
4. Duplicate Claim Submissions
Submitting the same claim more than once without following the correct resubmission procedure may result in a CO-252 denial.
5. Coverage or Eligibility Issues
If the patient’s insurance coverage wasn’t active on the date of service or benefits didn’t cover the billed procedure, the claim may be denied under CO-252.
Struggling with CO-252 denials? Contact Resilient MBS for expert guidance in resolving denials, ensuring compliance, and optimizing your revenue cycle.
Impact of CO-252 Denials on Healthcare Revenue
Even a single unresolved denial can have ripple effects across your organization. The CO-252 Denial Code impacts both financial stability and operational efficiency.
Financial Impact
- Delays reimbursement and cash flow
- Increases accounts receivable (A/R) management costs
- Leads to potential write-offs when claims exceed the timely filing limits
For small practices, this can mean difficulty meeting payroll, paying vendors, or investing in new technologies.
Operational Challenges
When billing staff spend excessive time fixing denials, productivity suffers. Delays in claim resubmission can slow down workflows, frustrate staff, and reduce patient satisfaction. Over time, unresolved denials can weaken a practice’s revenue integrity and compliance posture.
How to Fix CO-252 Denials (Step-by-Step Solution)
Resolving CO-252 denials requires a systematic and detail-oriented approach. Here’s how to get it right:
Step 1: Review the EOB (Explanation of Benefits)
Identify the exact reason for the denial. The EOB will specify whether missing documents, coding mismatches, or eligibility issues caused the CO-252.
Step 2: Verify Patient and Insurance Information
Double-check all patient demographics, insurance details, and responsibility sections in the claim form to ensure accuracy.
Step 3: Validate Coding and Billing Details
Ensure all CPT, HCPCS, and ICD-10 codes align with payer rules. Verify modifiers, units, and service dates are entered correctly.
Step 4: Re-Attach Supporting Documentation
Attach all necessary documents, physician notes, prior authorizations, medical necessity proofs, and consent forms before resubmission.
Step 5: Communicate with the Payer
Contact the payer to confirm what corrections are needed. Log all communications to build an audit trail for future reference.
How to Prevent CO-252 Denials
Prevention is more effective and less costly than correction. Implementing strong preventive measures ensures cleaner claims and faster reimbursements.
1. Implement Early Verification
Verify patient eligibility, coverage dates, and pre-authorization requirements before services are rendered.
2. Invest in Staff Training
Educate billing teams about common CO-252 denial causes and how to avoid them.
3. Leverage Automation and Analytics
Use automated claim scrubbing tools to detect missing or invalid information before submission. Denial management software can also help track and analyze denial trends for continuous improvement.
4. Regular Audits
Perform periodic audits of claims to identify recurring patterns of CO-252 denials and address root causes proactively.
5. Maintain Clear Communication
Encourage collaboration between billing, front-desk, and clinical teams to ensure documentation accuracy from start to finish.
When to Seek Expert Help
If your team continues facing frequent CO-252 denials despite process improvements, it might be time to bring in professionals.
Signs You Need Expert Support:
- High denial rates even after internal audits
- Staff are overwhelmed by rework and claim corrections
- Revenue cycle bottlenecks affecting cash flow
Why Choose Resilient MBS
At Resilient MBS, we specialize in denial management and revenue recovery. Our experts handle everything from denial root cause analysis to payer follow-up and claim resubmission. With our support, healthcare providers can:
- Reduce CO-252 and other denial occurrences
- Speed up reimbursements
- Maintain full compliance with payer guidelines
- Focus more on patient care, not paperwork
Final Thoughts
The CO-252 Denial Code might seem minor, but its repeated occurrence can lead to serious financial and operational strain. By understanding its causes, implementing preventive measures, and leveraging expert help, healthcare organizations can protect their revenue and streamline their billing process.
At Resilient MBS, we help practices not only fix CO-252 denials but also prevent them through data-driven denial management solutions.
Struggling with CO-252 denials?
Contact Resilient MBS today to schedule a free audit and discover how our experts can optimize your billing workflow, reduce denials, and accelerate your cash flow.
FAQs
What is the CO-252 Denial Code?
CO-252 Denial Code indicates a claim cannot be processed because of missing or incorrect patient responsibility information.
What causes CO-252 denials?
Common causes include coding errors, missing documents, payer rule violations, and inactive insurance coverage.
How can I fix CO-252 denials?
Review the EOB, correct errors, verify patient details, reattach missing documents, and resubmit the claim to the payer.
Can CO-252 denials be prevented?
Yes. Regular audits, proper documentation, automation tools, and staff training can help minimize these denials.
Who can help resolve CO-252 denials?
Resilient MBS offers expert denial management services to quickly identify and fix CO-252 issues, ensuring smooth revenue cycle operations.










