Medicare Modifiers may look like simple two-character add-ons, but they hold massive weight in medical billing. These modifiers communicate essential information about coverage, patient responsibility, ABN requirements, and whether a service should be paid or denied. When used inaccurately, they can trigger denials, repayment demands, audits, or compliance risks.
Among the wide range of Medicare modifiers, the GA modifier Medicare, GX modifier, GY modifier, and GZ modifier Medicare stand out as some of the most frequently misunderstood. They all relate to coverage restrictions, but each communicates a very different message to Medicare.
This comprehensive guide breaks down what each modifier means, when it must be used, and how it impacts reimbursement. You’ll also learn how the 25 modifier Medicare interacts with these modifiers and how to avoid the costly billing errors many practices unknowingly make.
What Are Medicare Modifiers?
Medicare Modifiers are short, two-letter/number codes appended to CPT and HCPCS codes to explain special circumstances surrounding a service. While the base CPT code describes what was done, the modifier clarifies how or why it was done, affecting:
- Claims processing
- Coverage eligibility
- Payment responsibility
- Compliance with Medicare rules
Using the correct modifier ensures your claims reflect accurate circumstances and prevent unnecessary denials.
Understanding the Key Medicare Modifiers: GA, GX, GY, and GZ
1. GA Modifier – Service May Not Be Covered (ABN Signed)
The GA modifier for Medicare is used when:
- A service may be denied by Medicare
- The provider expects Medicare non-coverage
- The patient has signed a valid Advance Beneficiary Notice (ABN) agreeing to pay if Medicare denies
This modifier signals:
“Medicare might not cover this. The patient has been informed and accepts financial responsibility.”
When to Use the GA Modifier
Use the GA modifier when:
- A service is potentially non-covered
- The provider believes denial is likely
- A properly completed ABN is on file before the service is furnished
Example
A patient requests a procedure that Medicare may consider routine or unnecessary. The provider obtains a signed ABN, then bills the service with the GA modifier to document patient awareness.
Best Practices
- Ensure ABNs are complete, current, and signed
- Never use GA without documentation
- Maintain clear logs of all ABNs
2. GX Modifier – Voluntary Notice for Non-Covered Services
The GX modifier Medicare is added when:
- A service is not covered by Medicare, based on program guidelines
- An ABN is voluntarily issued
- The patient chooses to receive the service, knowing Medicare will deny the claim
GX specifically communicates:
“This service is never covered. The patient was informed voluntarily.”
Common Use Cases
- Preventive tests outside the Medicare criteria
- Elective or optional procedures
- Screenings not indicated by age or diagnosis
Example
A patient requests an additional screening test not covered under their Medicare preventive schedule. The GX modifier shows the patient was informed and agreed to pay.
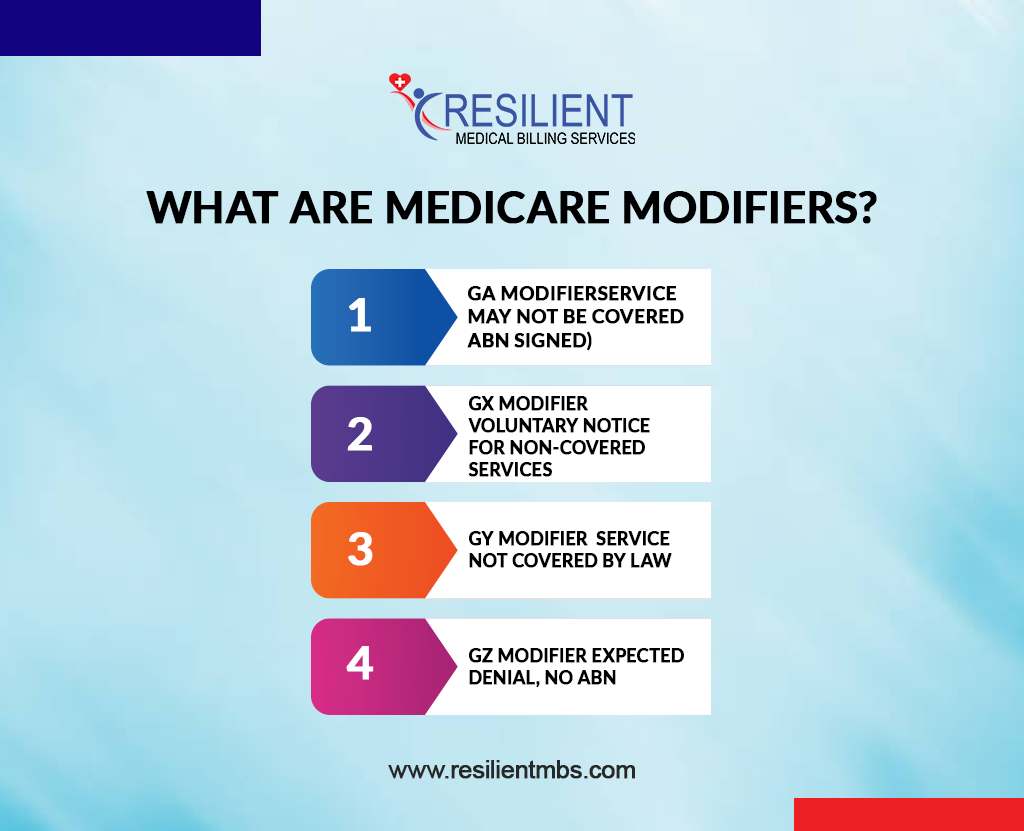
3. GY Modifier – Service Not Covered by Law
The GY modifier Medicare applies when:
- A service is statutorily excluded
- Medicare will never provide payment under any circumstances
- An ABN is not required
Examples include:
- Routine dental care
- Cosmetic services
- Durable medical equipment not meeting coverage requirements
Why the GY Modifier Matters
Failing to use the GY modifier can result in:
- Incorrect claim rejections
- Compliance flags
- Delays in patient billing
- Miscommunication with Medicare regarding exclusion status
This modifier cleanly communicates “This is not a Medicare benefit.”
4. GZ Modifier – Expected Denial, No ABN
The GZ modifier Medicare is used when:
- A service is likely to be denied
- An ABN was not obtained
- Medicare should automatically deny the claim
This modifier sends a clear message:
“Provider expected denial but did not issue an ABN.”
When GZ Must Be Used
Only use GZ when:
- Medical necessity cannot be supported
- Medicare non-coverage is highly likely
- ABN was not obtained (intentionally or unintentionally)
Important Clarification
GZ does not shift responsibility to the patient automatically.
Medicare typically pays nothing when GZ is used, and the provider may be responsible depending on state rules.
How These Modifiers Compare
| Modifier | Coverage Status | ABN Required? | Financial Responsibility |
| GA | Likely non-covered | Yes | Patient |
| GX | Not covered (voluntary) | Optional ABN | Patient |
| GY | Statutorily excluded | No | Patient |
| GZ | Expected denial, no ABN | No | Usually provider |
Understanding these distinctions is crucial for clean, compliant Medicare claims.
Using Modifier 25 with GA, GX, GY, and GZ
The 25 modifier Medicare indicates:
A separately identifiable and significant E/M service provided on the same day as a procedure.
Modifier 25 can be used with GA, GX, GY, or GZ when:
- A distinct E/M service is performed
- Documentation supports an unrelated or additional service
- Both services meet Medicare billing criteria
Examples
- GA + 25: ABN signed + separate E/M
- GX + 25: Non-covered service + distinct exam
- GY + 25: Statutorily excluded service + medically necessary E/M
- GZ + 25: Expected denial service + separate documented assessment
Correct pairing prevents denials and demonstrates clear service separation.
Need Medicare Modifier Expertise?
Contact Resilient MBS today for clean, compliant, and denial-free medical billing.
Common Errors to Avoid
Even experienced billers make mistakes. Avoid these pitfalls:
Misusing Modifier 25
Adding modifier 25 for minor visits or routine pre-procedure checks is inappropriate.
Missing ABN Documentation
Using GA without a signed ABN is a compliance violation.
Incorrect Modifier Combinations
Pairing modifiers incorrectly can lead to rejected claims.
Poor Documentation
Insufficient notes fail to justify modifier use and can result in audits.
Tips for Accurate Medicare Modifier Billing
- Always verify whether the service is covered, non-covered, or excluded
- Maintain clear ABN documentation for GA
- Use GX only for voluntary notices
- Apply GY to statutorily excluded services
- Use GZ when denial is expected and no ABN is present
- Conduct internal audits regularly
- Train staff on Medicare modifier distinctions
Accurate modifier usage ensures smoother claims, fewer denials, and improved compliance.
Conclusion
Using Medicare Modifiers GA, GX, GY, and GZ correctly is essential for clean claim submission, regulatory compliance, and proper reimbursement. Each modifier carries a specific message about coverage, patient responsibility, and ABN requirements. When paired with accurate documentation and appropriate use of the 25 modifier, providers can minimize denials and ensure clear communication with Medicare.
If your practice struggles with Medicare modifier usage or compliance, Resilient MBS can help. Our specialists ensure accurate claim submission, proper modifier application, and maximum reimbursement.
FAQs
What are Medicare Modifiers and why are they important?
Medicare Modifiers provide additional details about a service, helping Medicare determine coverage, payment, and responsibility.
When should the GA modifier Medicare be used?
Use GA when a patient signs an ABN indicating they understand Medicare may deny the service.
How is GX different from GA?
GX is for services Medicare never covers, while GA is for services Medicare may deny with an ABN.
What do GY and GZ modifiers mean?
- GY: Service not covered by law
- GZ: Service expected to be denied, no ABN on file
Can modifier 25 be used with GA, GX, GY, or GZ?
Yes, when a significant, separate E/M service is documented on the same day.










