In healthcare, one crucial question defines trust: Can you rely on the person caring for you?
Every medical professional’s qualifications directly influence patient safety, treatment quality, and overall confidence in healthcare systems. That’s why credentialing and privileging in healthcare are two foundational processes that ensure each provider is both competent and authorized to deliver care safely.
At Resilient MBS, we specialize in helping healthcare organizations streamline these complex procedures; ensuring compliance, minimizing delays, and protecting both providers and patients.
Let’s explore what credentialing and privileging mean, how they differ, and why they’re essential to maintaining quality and trust in modern healthcare.
What Is Credentialing in Healthcare?
Credentialing in healthcare is the formal process of verifying a provider’s qualifications, including their education, training, licenses, certifications, and clinical experience, to ensure they meet recognized professional standards.
During this process, healthcare organizations or payer networks confirm the provider’s background directly from primary sources such as:
- Medical and nursing schools
- State licensing boards
- Certification agencies
- Previous employers and references
Credentialing also includes checking for any history of disciplinary actions, malpractice claims, or sanctions, ensuring patient safety and regulatory compliance.
Why It Matters:
Credentialing protects patients from unqualified or fraudulent providers, ensures organizations meet federal and state compliance standards, and supports eligibility for insurance reimbursements. It also safeguards a healthcare facility’s reputation and accreditation.
Learn more about provider credentialing services to ensure compliance and patient safety.
What Is Privileging in Healthcare?
While credentialing confirms a provider’s qualifications, privileging in healthcare determines what specific clinical procedures or services they are authorized to perform based on their verified skills and experience.
Typically, a hospital’s medical staff committee reviews the provider’s specialty, training, and performance before granting privileges. These privileges may include:
- Performing surgeries
- Administering anesthesia
- Conducting diagnostic imaging
- Managing specialized therapies or treatments
By defining the exact scope of clinical practice, provider privileging ensures that only properly trained professionals perform advanced procedures, reducing medical risks and improving patient outcomes.
The Credentialing and Privileging Process
Both processes work together to maintain healthcare safety, compliance, and efficiency. Here’s a closer look at how they function step-by-step:
Step 1: Credentialing – Verification of Qualifications
This stage involves thorough background verification, including:
- Education and degree validation
- License and certification verification
- Work history, references, and malpractice review
Healthcare organizations may perform these checks manually or use credentialing management software to automate the process, avoid errors, and ensure faster turnarounds. Many facilities also outsource to credentialing specialists like Resilient MBS for reliable, compliant results.
Step 2: Privileging – Authorization for Specific Care
Once a provider is credentialed, the organization reviews their competencies and grants privileges for specific procedures or treatments.
For example, a cardiologist might receive privileges for performing echocardiograms but not for open-heart surgery, unless their credentials justify it.
Reappointment and Renewal
Provider Credentialing and privileging are not one-time events. Most healthcare facilities re-evaluate providers every 2–3 years to confirm that credentials remain current and clinical competencies are maintained. This includes checking for license renewals, continuing education, and any disciplinary actions.
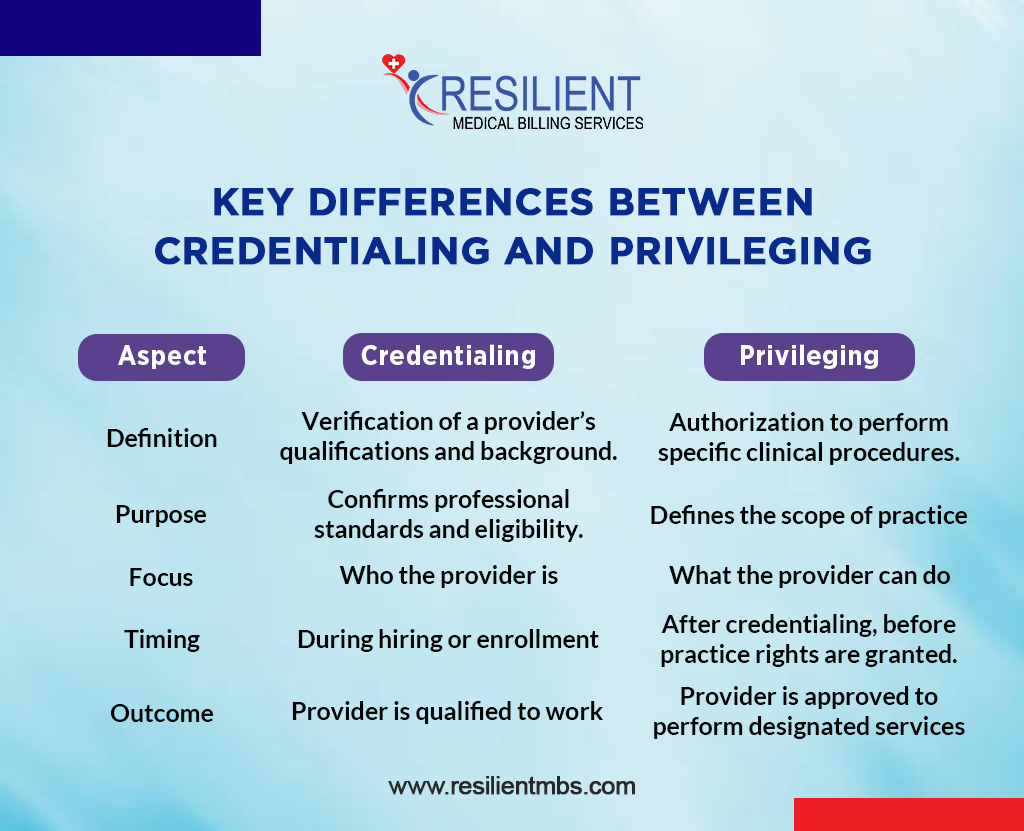
Key Differences Between Credentialing and Privileging
| Aspect | Credentialing | Privileging |
| Definition | Verification of a provider’s qualifications and background. | Authorization to perform specific clinical procedures. |
| Purpose | Confirms professional standards and eligibility. | Defines the scope of practice. |
| Focus | Who the provider is. | What the provider can do. |
| Timing | During hiring or enrollment. | After credentialing, before practice rights are granted. |
| Outcome | Provider is qualified to work. | Provider is approved to perform designated services. |
Summary: Credentialing confirms competence, while privileging defines permission. Both ensure patients receive safe, high-quality care.
Why Credentialing and Privileging Matter in Healthcare
Credentialing and privileging are not just compliance requirements; they are core pillars of patient safety and quality care.
These processes ensure that:
- Providers meet state and federal professional standards.
- Hospitals maintain accreditation and insurance eligibility.
- Patient safety is prioritized through competence-based authorization.
- Errors, lawsuits, and malpractice risks are minimized.
Failure to maintain up-to-date credentialing or privileging can lead to denied claims, regulatory fines, or loss of accreditation, outcomes that no healthcare organization can afford.
Need help with provider verification? Contact Resilient MBS to streamline your credentialing and privileging workflow.
Common Challenges and Best Practices
Managing credentialing manually often leads to delays, missing documents, and compliance risks. Healthcare facilities face challenges like:
- Time-consuming verification.
- Frequent regulation updates.
- Risk of data errors.
Best Practices Include:
- Using automated credentialing software to track expiration dates and renewals.
- Partnering with credentialing experts for faster and accurate verification.
- Maintaining secure digital records to prevent data loss.
Resilient MBS offers customized credentialing and privileging solutions to help healthcare providers save time, stay compliant, and focus on patient care. Schedule a consultation with our credentialing specialists today to simplify your provider verification process.
Final Words
Credentialing and privileging in healthcare form the backbone of patient safety and trust. They verify qualifications, define responsibilities, and ensure compliance across every level of care.
At Resilient MBS, we help healthcare organizations simplify these processes with professional credentialing services, digital solutions, and expert support, ensuring compliance, accuracy, and efficiency every step of the way.
Ready to improve your credentialing workflow? Book a free consultation with Resilient MBS today.
FAQs
What is the purpose of credentialing in healthcare?
Credentialing verifies a provider’s qualifications, ensuring they are properly trained and licensed to deliver safe care.
Who manages the credentialing and privileging process?
Typically, a hospital’s medical staff office or credentialing committee handles verification and approval.
How often should privileging be renewed?
Usually, every 1–2 years, depending on institutional policies and state requirements.
Can credentialing and privileging be done online?
Yes. Many organizations use secure, cloud-based systems for faster and more accurate credentialing management.
What is the difference between credentialing and privileging in healthcare?
Credentialing verifies a provider’s qualifications and licenses, while privileging authorizes specific medical procedures that they are allowed to perform.










