Medical billing is more than just paperwork; it’s the engine that drives healthcare revenue. At its core lies coding, which translates patient care into standardised formats for insurance claims and reimbursement. But when codes don’t match the complexity of services provided, it can quietly cost providers thousands.
This issue is known as downcoding. A standard yet often overlooked error is where lower-level codes are submitted, resulting in reduced payments and potential compliance risks.
For healthcare organisations seeking to enhance their Revenue Cycle Management (RCM), recognising and addressing downcoding is crucial. Accurate coding isn’t just about compliance; it’s about ensuring fair reimbursement for the care delivered.
Why Downcoding Matters in Medical Billing
Downcoding, the practice of assigning a lower-level billing code than the service warrants, is a critical issue in medical billing. Often caused by vague documentation or coding oversights, it can result in underpayment, misrepresentation of services, and compliance concerns.
Understanding the effects of downcoding encourages healthcare providers to enhance their clinical documentation and ensure accurate coding. By addressing downcoding early, practices can protect their revenue, avoid audit risks, and promote accuracy and integrity across the billing process.
What is Downcoding?
Downcoding Medical Definition
Downcoding in medical billing refers to the assignment of a healthcare service code that represents a lower level of complexity or cost than what was provided. This coding discrepancy typically results in reduced reimbursement from payers.
Difference Between Upcoding and Downcoding
While both upcoding and downcoding involve inaccuracies in medical coding, they are opposite:
Upcoding refers to assigning a higher-level or more expensive code than the service performed, which can often trigger audits and compliance scrutiny due to potential concerns about fraud.
Downcoding, on the other hand, involves assigning a lower-level code than appropriate, leading to underpayment for services and diminished practice revenue.
Both upcoding and downcoding make RCM very hard to use and may negatively impact compliance. However, downcoding is especially problematic when it occurs due to changes made by a third-party customer rather than the provider’s intended purpose.
Common Types of Downcoding
Downcoding in medical billing involves assigning a lower-level code than warranted by documented services, leading to reduced reimbursement and financial losses. It often results from errors or procedural inconsistencies within the healthcare system.
- Manual Coding Errors
The first type of downcoding is coding errors. Manual downcoding occurs when coders unintentionally assign lower-level codes due to oversight or misinterpretation of clinical documentation. This often stems from unfamiliarity with CPT guidelines or misjudging the complexity of services, leading to revenue loss and compliance risks.
- Automated System Errors
Automated coding tools and EHRs can downcode claims due to misclassified data or flawed algorithms. These systems require regular audits to ensure coding accuracy and alignment with clinical documentation.
- Payer-Initiated Downcoding
Insurance payers can downcode claims if they believe the documentation doesn’t support the billed service level. This often occurs without provider input, resulting in delayed payments and an increased administrative workload due to the appeal process.
Why Downcoding Happens
To keep the revenue cycle running smoothly and comply with the rules, it’s essential to understand the root cause of downcoding.
One major factor is documentation deficiencies. When clinical records lack detail or completeness, coders may default to lower-level codes, which can result in claims being rejected. Ambiguous clinical notes also contribute, as vague language can hinder accurate code assignment.
Another common issue is insufficient coder training; without proper knowledge of coding rules and payer policies, coders may choose conservative codes.
Additionally, insurance payers’ audit practices can lead to downcoding, mainly when they apply proprietary guidelines that override provider documentation. Addressing these issues through clear documentation, coder education, and proactive claim management is key to minimising downcoding.
The Impact of Downcoding on RCM
Downcoding significantly harms Revenue Cycle Management (RCM). While some believe it avoids payer scrutiny, downcoding can increase reimbursements, but it ultimately reduces revenue and increases compliance risks.
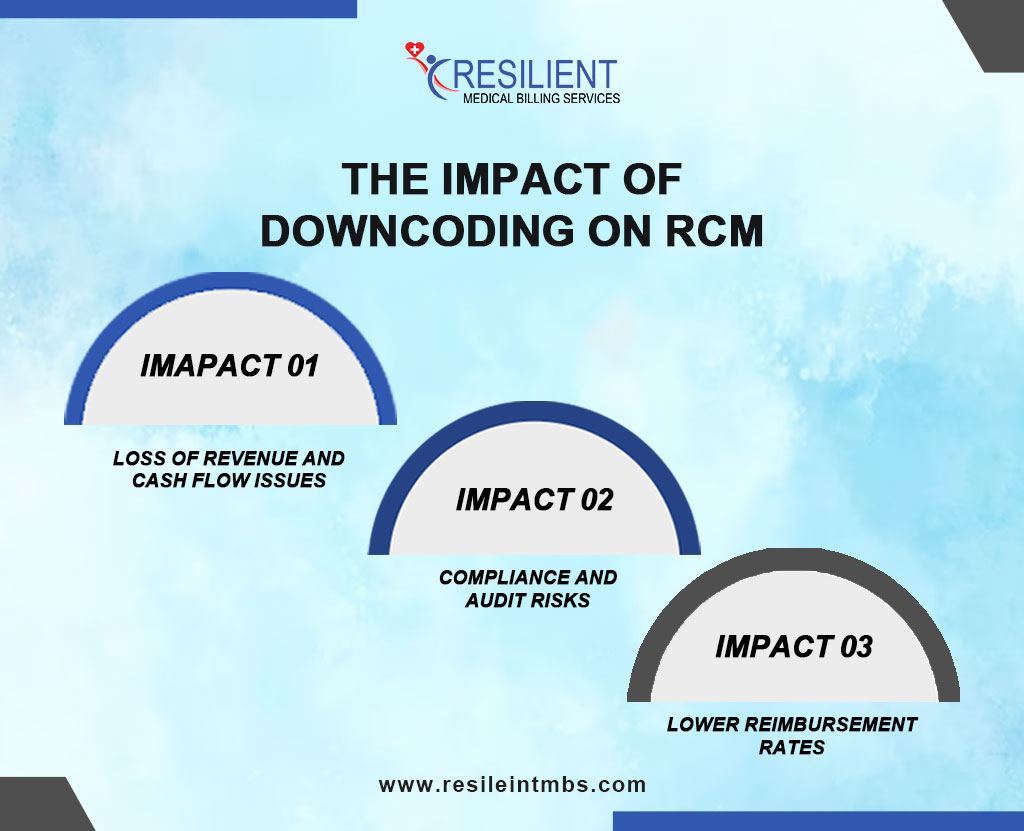
Loss of Revenue and Cash Flow Issues
Billing at lower service levels than provided results in underpayment. This leads to discrepancies between expected and actual revenue, resulting in cash flow problems, particularly for smaller or specialised practices.
Compliance and Audit Risks
Though intended to avoid denials, downcoding can raise compliance concerns. Frequent underreporting may trigger audits, as payers view it as improper billing, which could lead to fines under laws such as the False Claims Act.
Lower Reimbursement Rates
Downcoding leads to consistent undercompensation. It distorts payer data and may negatively influence future contract negotiations and reimbursement models.
How to Prevent/ Avoid Downcoding in Medical Billing
To protect revenue, maintain RCM transparently, and ensure legal compliance, it’s crucial to stop downcoding.
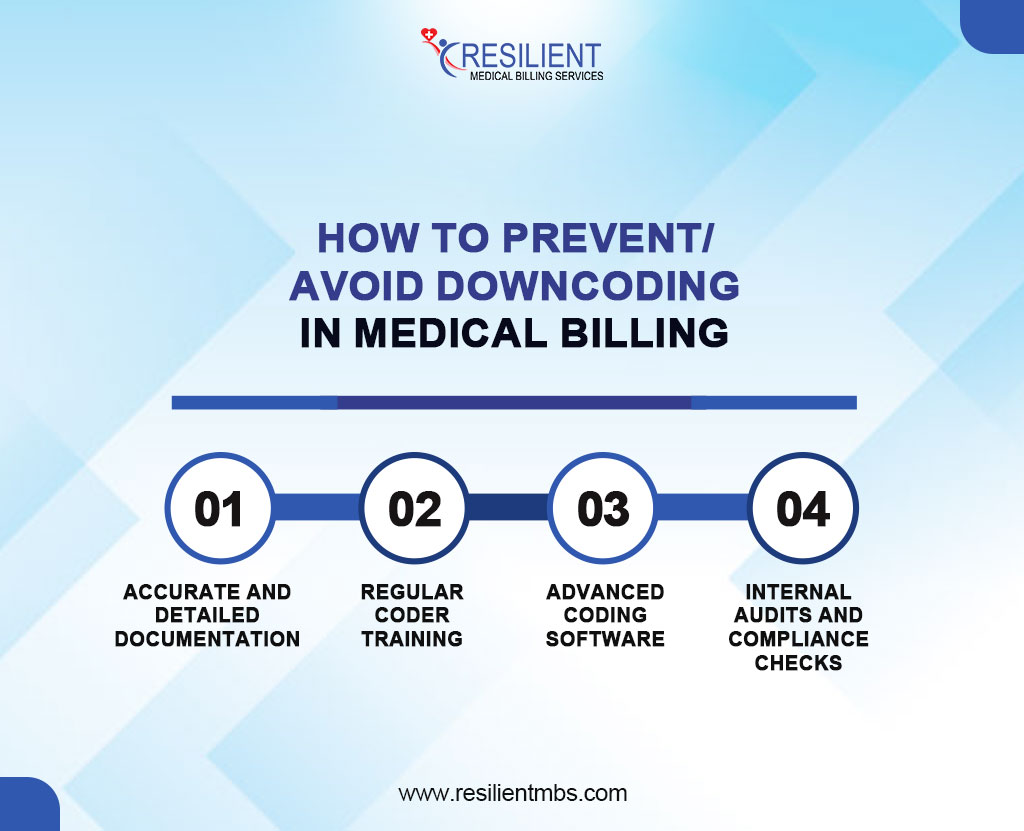
Key strategies for how to prevent downcoding include:
- Accurate and Detailed Documentation
Thorough clinical documentation, covering symptoms, treatments, procedures, and outcomes, ensures accurate code assignment and supports the billed level of care.
- Regular Coder Training
Ongoing education keeps coders up to date with evolving CMS guidelines and coding standards, reducing errors and reinforcing best practices.
- Advanced Coding Software
Using Computer-Assisted Coding (CAC) tools enhances accuracy by analysing documentation and suggesting appropriate codes, minimising human error, and improving consistency.
- Internal Audits and Compliance Checks
Regular audits identify downcoding trends, flag inconsistencies, and provide insights to improve billing practices and coder performance.
Steps to Prevent Downcoding in Medical Billing
- Educate healthcare providers on proper documentation practices to support accurate medical coding.
- Perform regular coding audits monthly or quarterly to identify and correct errors.
- Promote real-time communication between coders and clinicians to resolve unclear or incomplete documentation.
- When necessary, bring in external experts to conduct unbiased compliance reviews.
- Establish uniform coding procedures throughout all departments to ensure consistency.
- Educate healthcare providers on proper documentation practices to support accurate medical coding.
- Perform regular coding audits, monthly or quarterly, to identify and correct errors.
- Promote real-time communication between coders and clinicians to resolve unclear or incomplete documentation.
- Establish uniform coding procedures throughout all departments to ensure consistency.
Closing Words
Downcoding in medical billing, whether intentional or accidental, can severely impact revenue, compliance, and the accuracy of patient care records.
To safeguard Revenue Cycle Management (RCM), healthcare providers must prioritise thorough documentation, invest in coder training, conduct regular audits, and leverage innovative billing technologies.
A proactive and informed approach ensures accurate reimbursements, strengthening both financial stability and care integrity.
For expert support in identifying and preventing downcoding issues, contact Resilient MBS today. Our team of experienced billing professionals is here to help you protect your revenue and ensure full compliance with current coding standards.










