Ever wondered why your hospital bill looks like a jungle of codes and charges? Or why does it take so long for insurance to process your claim?
Behind every hospital visit is a complex system working to make sure providers get paid and patients aren’t left in the dark.
Hospital medical billing plays a vital role in keeping the healthcare system running. It makes sure hospitals get paid for the care they give, and when everything is done right, it’s beneficial to everyone. For patients, it means fewer surprises and more clarity about what they owe. For providers, it means faster reimbursements and fewer claim denials.
We’ll take the mystery out of hospital medical bills, look at how it works, and talk about why it’s more important than ever to understand it.
What is Hospital Medical Billing?
Hospital medical billing refers to the process through which healthcare facilities document, submit, and follow up on claims with health insurance companies to receive healthcare bill payment for medical services rendered to patients. This procedure includes capturing patient information, assigning standardized medical codes for diagnoses and procedures, and transmitting claims for reimbursement.
The Worth of a Competent Hospital Billing System
The hospital billing department handles tasks like patient registration, insurance verification, coding, charge capture, and accounts receivable management. Billing specialists ensure that claims are accurate, complete, and follow payer guidelines.
They also manage claim rejections, process payments, and assist patients with billing or insurance questions. A well-organized billing system is crucial for maintaining the hospital’s cash flow and ensuring patient satisfaction with clear, accurate billing.
The Medical Billing Process And Procedures
The medical billing cycle ensures healthcare providers receive timely reimbursement for services.
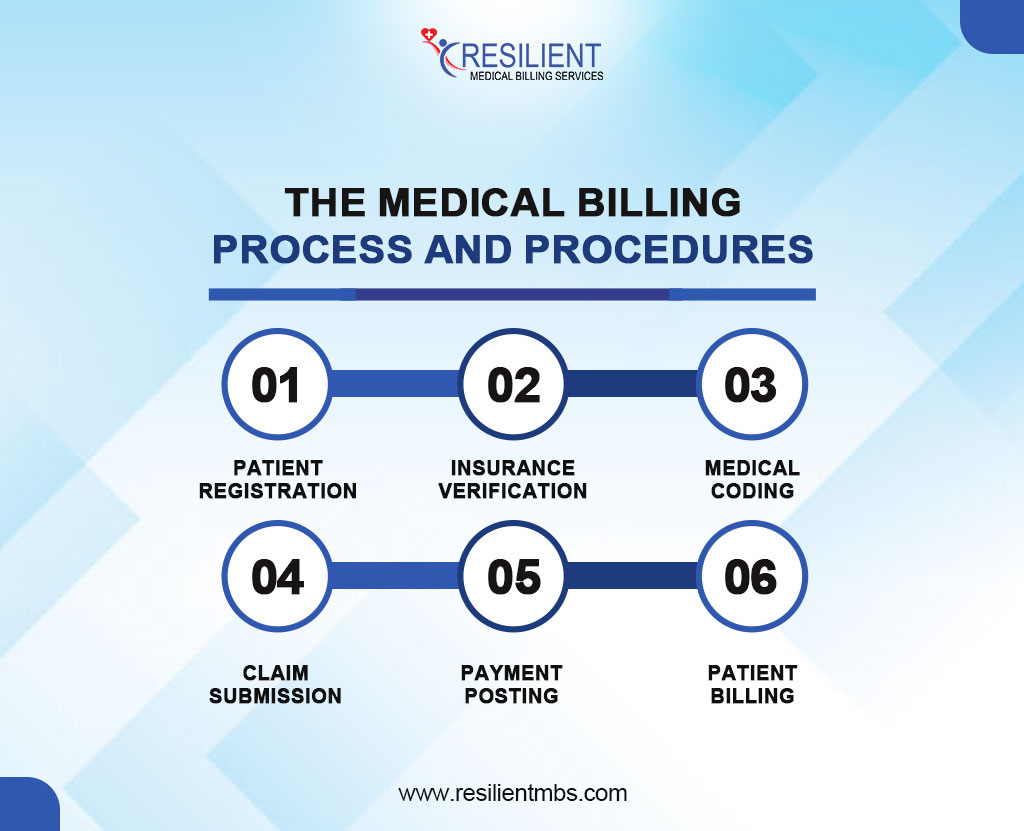
Below are key medical billing cycle steps that require accuracy and compliance:
- Patient Registration: Collects demographic and insurance info to ensure proper identification and billing. Errors can lead to claim delays or rejections.
- Insurance Verification: Verifies patient coverage and eligibility to avoid denials and unexpected costs.
- Medical Coding: Translates diagnoses and services into standardized codes (ICD-10, CPT, HCPCS). Accurate coding is crucial for compliance and reimbursement.
- Claim Submission: Submits claims to insurers following payer-specific standards. Timely submission ensures meeting deadlines.
- Payment Posting: Posts insurer payments to the patient’s account, adjusting for contractual obligations and identifying any remaining balance.
- Patient Billing: Bills patients for any outstanding balance, providing clear, itemized statements and convenient payment options.
Each step is essential to reducing claim denials, improving cash flow, and building patient trust. Inaccuracies or delays at any stage can lead to financial losses
Key Terms Explained
CPT Codes: These are five-digit numeric codes used to describe medical, surgical, and diagnostic services for billing purposes.
ICD-10 Codes: These alphanumeric codes represent diagnoses and are used globally for statistical and billing purposes.
EOB (Explanation of Benefits): A document sent by insurers outlining what portion of the claim was paid and any patient responsibility.
Deductible: The amount a patient must pay out of pocket before insurance begins to cover services.
Co-pay and Co-insurance: Fixed amounts or percentages patients pay for services after insurance processes the claim.
How Do Hospital Bills Work?
Inpatient and outpatient claims are handled by hospital bills, which start with verifying the patient and their insurance. Services are written down, coded, and given prices, and claims are sent in using UB-04 forms to get paid back. For proper billing and safety, accurate coding is a must. Denials or delays can happen because of mistakes. Patients, doctors, and insurers all work together on the process to make sure it is efficient and accurate.
Payment Of Hospital Bill
Hospital bill payment is a structured process through which healthcare providers collect fees for medical services rendered to patients. Transparency and financial preparation require knowledge of patient billing and payment mechanisms. After getting care, patients receive a complete invoice listing all services and expenditures. This fee covers doctor visits, diagnostic testing, drugs, surgery, and lodging.
Methods of Hospital Bill Payment
Hospitals typically offer several payment methods to accommodate diverse patient preferences and financial capabilities. Common options are:
Online Payment Portals: Secure hospital websites or third-party platforms allow patients to pay bills electronically.
In-person Payments: Payments are made directly at the hospital’s billing department via cash, check, or card.
Payment Plans: Structured installment plans for patients facing financial constraints.
Phone Payments: Billing representatives can process payments over the phone.
Role of Insurance and Out-of-Pocket Costs
Health insurance determines how much of a hospital bill is paid. After treatment, the hospital sends a claim to the insurer, which covers part of the cost. The patient is responsible for the rest, including deductibles and copayments. Uninsured patients must pay the full amount unless financial aid is offered.
Comprehensive hospital bill insurance reduces out-of-pocket costs, while limited or high-deductible plans can increase them. Patients should understand their policy to avoid unexpected charges.
Common Issues with Hospital Billing
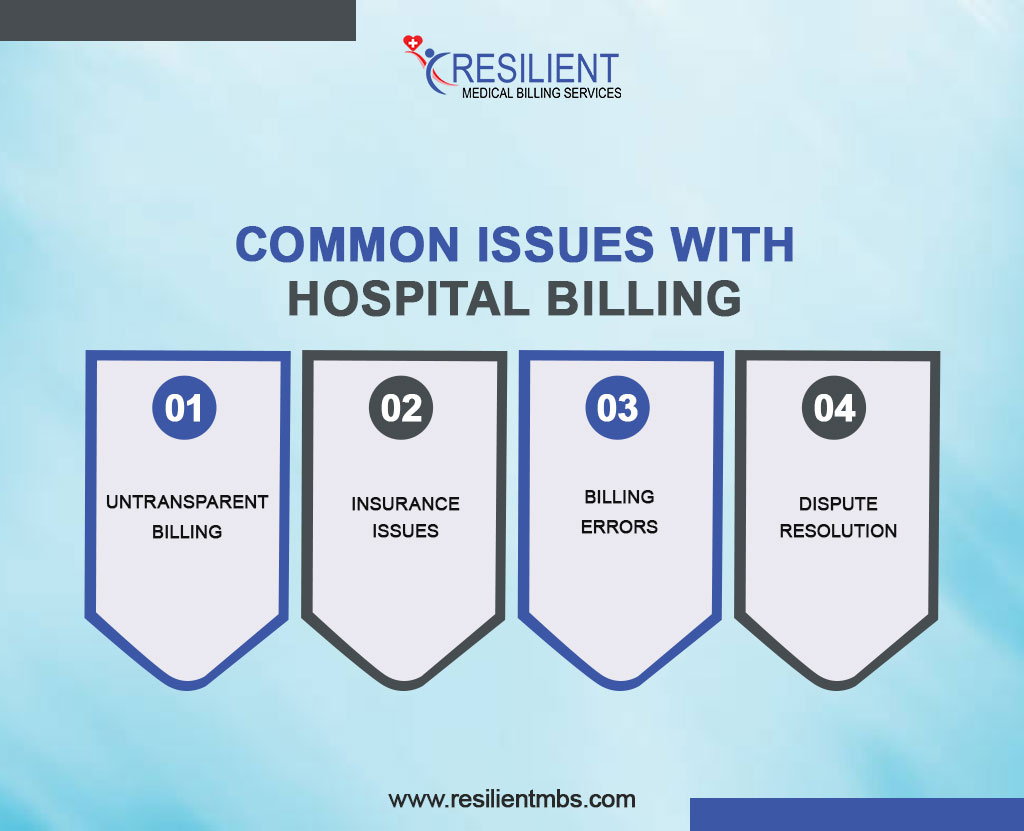
- Untransparent billing: This causes disagreements due to unclear itemizations and cost differences.
- Insurance issues: Delays, incomplete reimbursements, and denials affect patient care and revenue cycles.
- Billing errors: Coding errors and erroneous patient info delay payments.
- Dispute Resolution: Patients should review bills, contact billing, and obtain a written review. A billing advocate or lawyer may aid with complex cases.
How to Avoid Surprise Hospital Bills
Surprise medical bills often occur when patients unknowingly receive care from out-of-network providers, particularly during emergencies or hospital stays. These unexpected charges can be financially burdensome, even for those with insurance.
Preventative Measures
To avoid surprise bills, patients should verify insurance coverage beforehand. This includes confirming if hospitals, doctors, anesthesiologists, and labs are in-network. Patients can use online directories, contact their insurance provider, or speak with the hospital’s billing office for confirmation.
For elective care, patients should request a written cost estimate, including out-of-pocket expenses, and ensure pre-authorization is in place. Seeking in-network referrals for follow-up services can also help prevent unexpected charges.
Concluding Words
Understanding the hospital medical billing process is crucial for both patients and providers. From registration to final payment, each step ensures accurate and transparent billing. Knowing how hospital bills and insurance work helps patients avoid confusion and financial strain.
Why understanding the billing process matters:
- Helps identify billing errors and discrepancies.
- Enables better communication with healthcare providers.
- Improves management of healthcare expenses.
- Reduces the risk of unexpected charges.
What patients can do:
- Learn the steps in the hospital billing cycle.
- Understand your insurance coverage and responsibilities.
- Ask questions about unclear charges or procedures.
- Review all medical bills carefully before making payments.
Need expert help?
Contact Resilient MBS for professional guidance and support to simplify your hospital medical billing experience and ensure accuracy every step of the way.










