Claim types are necessary for the complex reality of medical billing processes to deliver accurate and timely reimbursement. Further, it is significant to note the importance of institutional claims for hospital and nursing home services when it comes to recovering from a PCDL.
It is estimable that these claims contributed to a significant proportion of the $3. Healthcare spending of $8 trillion, says CMS. These claims guarantee the facilities considerable reimbursement for offering such a plethora of services.
Institutional claims cover outpatient procedures and treatments as well as inpatient hospital stays, which make up roughly 20% of healthcare spending in 2022. The claims must be understood for effective reimbursement and regulatory compliance. Incomplete claims can cost a lot of money and potentially get you fined.
This blog will cover institutional claims, the UB-04 claim form, medical claim processing, and institutional vs. professional claims. You’ll learn how to manage claims and maximize revenue by the end.
What Are Institutional Claims?
Institutional claims are claims for services provided by institutional healthcare providers, such as hospitals, nursing facilities, and outpatient clinics. These claims are typically submitted on the UB-04 form.
Examples of Institutional Claims
Examples of institutions include hospital stays, surgical procedures, diagnostic tests as well as other non-institutional healthcare services dispensed by the healthcare institutions.
Why Institutional Claims Are Important in the Healthcare Industry
Institutional Claims vs Professional Claims
Institutional claims come from hospitals and other healthcare providers while personal claims are filled out by private service providers such as doctors and therapists.
In the institution and personal claims, one is important as the first deals with the activities in the facility, and the second deals with private service providers. Claims from institutions usually follow along the UB04 line, and professional claims follow the CMS1500 form.
The reimbursement frameworks and the claims processing arrangements for these claims have significant deviations as compared to those for professional claims. Health institution claims that need to be supported with proper documents generally should meet certain codes and billing requirements set by a medical stipulation.
Impact of Claim Type on Reimbursement and Documentation
The type of claim submitted can impact reimbursement rates and documentation requirements. These claims can be reimbursed differently than professional claims, and providers must ensure that they meet all documentation requirements to avoid claim denials or delays.
What Is the UB-04 Claim Form?
Purpose and Importance
The UB-04 claim form is used as the main aim to speed up an institutional medicine initiation billing system. These health providers include hospitals, care centers, transaction facilities, and other similar providers. It is a complete charge memorandum that has all the relevant details required for claim handling.
The UB-04 Claim Form
The UB-04 claim form holds various sections and areas that are required to be supplied with all their requisite information in order to clear all the relevant claims.
Some of the key components of the form include:
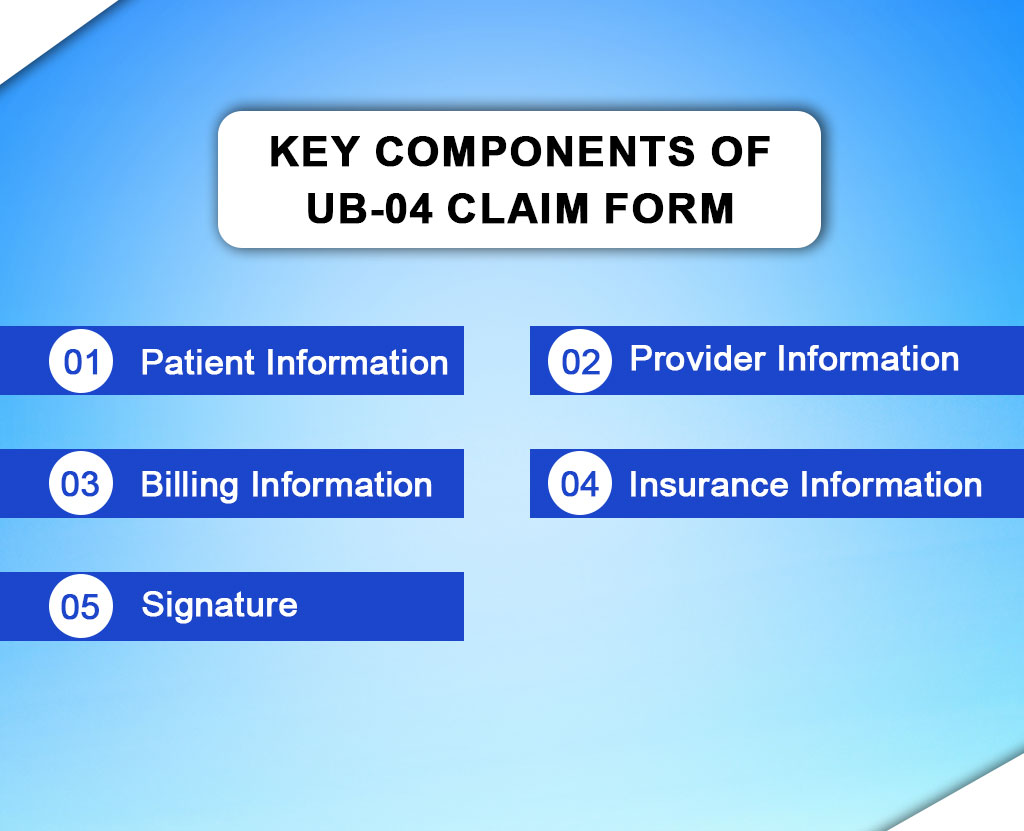
Patient Information
This area is where the patient’s essential information will be found. This includes the patient’s name, date of birth, and insurance information.
Provider Information
Here, an individual willing to provide health care services indicates himself/herself ensuring a simple introduction of their data which includes their name, address, and NPI.
Billing Information
In this section, you specify the services delivered wherein dates of service, procedures performed, and diagnosis codes are stated in detail.
Insurance Information
Providers need to provide the applicant’s primary and secondary insurance details as well.
Signature
There must be the signature of a responsible person on the form which is proof that the information is exact and the medical service was required.
Medical Claim Processing
Medical claim processing means that medical providers and insurance groups carry out or participate in the handling and approval of claims for services that they have given to patients. This is done using a combination of tasks, which employs the fullness, correctness, and promptness of claims.
How UB-04 Claim Forms are Used in the Medical Claim Process
The latest UB-04 forms have been designed to meet the institutional claims i. e. , the respective claims from the hospitals, nursing homes, etc. These forms would normally have fields with detailed information concerning the provision of services, such as dates, the process done, and diagnosis codes included. UB-04 forms are presented to insurance companies or other payers to seek reimbursement.
Steps Involved in Processing a UB-04 Claim Form
Data Entry
The provider or billing staff enters the relevant information from the patient’s visit into the UB-04 form.
Coding
Diagnosis and procedure codes are assigned based on the services provided.
Claim Submission
The completed UB-04 form is submitted to the insurance company or payer for processing.
Adjudication
The insurance company reviews the claim to determine coverage and reimbursement amount.
Payment
If the claim is approved, the insurance company issues payment to the healthcare provider.
Last thoughts from Resilient MBS
Knowing how to properly complete the UB-04 form and taking care to follow claim processing standards prevents institutions from frequently receiving denied or delayed payments.
The medical billing industry is dynamic and new practices and criteria should be reflected and implemented. Education, learning ongoing updates, and being up-to-date with billing legislation and coding will help billing professionals reduce errors and maintain compliance.
Automated billing solutions and periodic auditing also enhance billing procedures’ accuracy and efficiency.
Healthcare providers need proper claim submission, and Resilient MBS understands. We provide excellent medical billing audit services to help healthcare providers maximize reimbursements and reduce billing errors. Resilient lets healthcare practitioners focus on patient care while trusting Resilient to handle billing.










