Family medicine is at the heart of modern healthcare because it helps people and families at all times of their lives by giving them personalized, ongoing care. As the demand for easy access to preventive care rises, so does the need to make sure that the people providing it are competent.
Medical Credentialing is an important part of this process because it verifies a provider’s skills, lets insurance companies work with them, and builds trust between patients and providers.
For family medicine doctors, getting the right medical credentials is important for meeting industry standards and making sure patients get reliable, high-quality care.
What Is a Family Medicine Physician?
A family medicine physician is a medical doctor trained to provide comprehensive health care for people of all ages, from newborns to the elderly. These providers diagnose and treat a broad range of conditions, manage chronic diseases, offer preventive care, and often serve as the first point of contact in the healthcare system. Their training includes pediatrics, internal medicine, obstetrics and gynecology, psychiatry, and geriatrics, making them uniquely equipped to manage the diverse needs of entire families.
One common question patients and new providers ask is:
What is the difference between family medicine and internal medicine?
The Answer is Both specialties fall under primary care, yet the difference between family medicine and internal medicine is that internal medicine physicians focus solely on adult care, often in inpatient settings or subspecializing in fields like cardiology or endocrinology.
In contrast, family medicine physicians provide outpatient care to both children and adults and emphasize continuity of care over a patient’s lifetime.
The Role of Medical Credentialing Services
Medical credentialing services are very important for family medicine practices because they make sure that doctors have the right credentials, licenses, and experience to meet the standards set by insurers and government agencies.
Proper credentialing supports network involvement, guarantees compliance, and lets payers sign contracts. Without it, doctors could lose their payments and have fewer patients who can see them. Credentialing also encourages on-time payments and helps practices grow by letting them join PPOs, HMOs, and other insurance networks.
Process Of Credentialing
The credentialing process is a detailed and structured procedure that ensures healthcare providers meet industry standards and can deliver safe, quality care.
The process includes the following steps:
- Collection of essential documents, such as:
- Medical licenses
- Board certifications
- Malpractice insurance
- Hospital privileges
- Complete work history
- Primary source verification of all submitted documents to confirm their authenticity.
- Additional screening procedures, which may involve:
- Comprehensive background checks
- Peer references
- Completion of insurance panel-specific applications
- Final evaluation: to ensure the provider meets compliance requirements and industry standards.
- Outcome: A thoroughly vetted provider approved to deliver safe and effective patient care.
Benefits of Medical Billing and Credentialing Services for Family Physicians
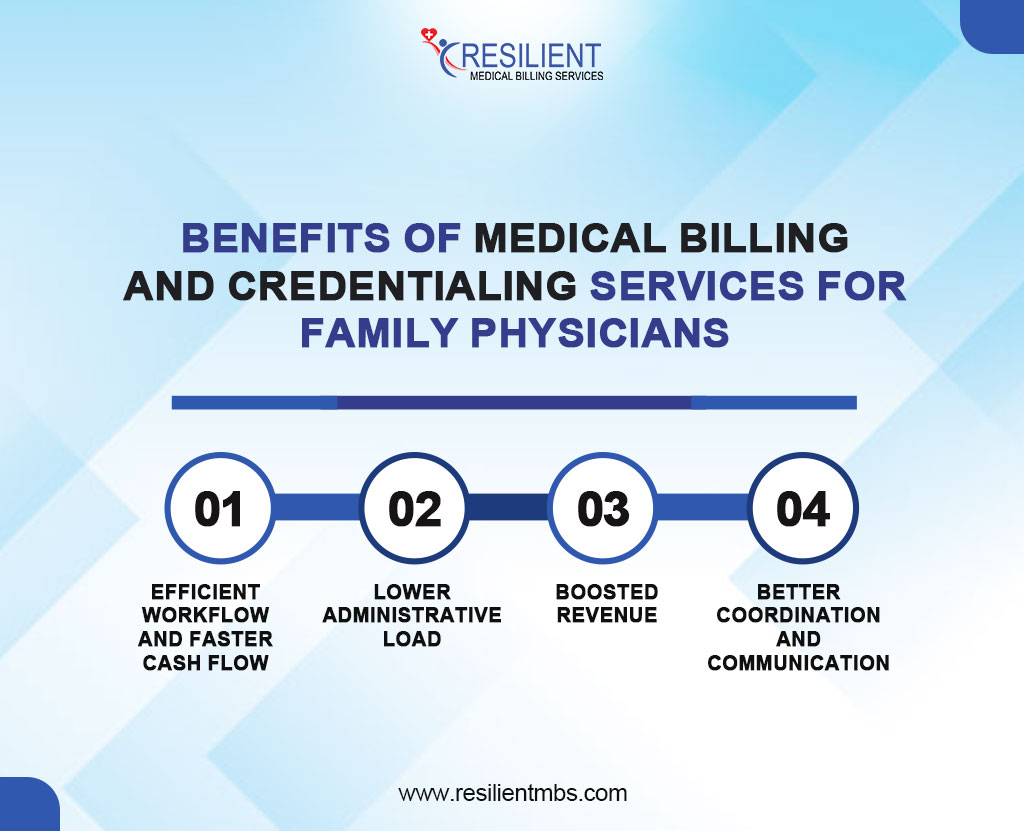
- Efficient Workflow and Faster Cash Flow
By involving billing and credentialing, practices minimize errors, avoid delays, and enable providers to start billing right after credentialing, enhancing cash flow.
- Lower Administrative Load
Outsourcing these tasks frees up time for staff to focus on patient care, improving satisfaction and overall practice operations.
- Boosted Revenue
Accurate billing and proper credentialing prevent claim denials and ensure quicker payments, leading to stronger revenue and financial health.
- Better Coordination and Communication
Managing both services together fosters smooth coordination, quicker issue resolution, and a steady revenue stream, ensuring efficient provider onboarding.
Understanding Medical Insurance Credentialing Services
Credentialing can be a complex and time-consuming process involving substantial paperwork and coordination with insurance payers. Outsourcing credentialing services makes the process easier by taking care of the paperwork, following up on applications, and making sure they are processed on time, so family practices can focus on giving their patients good care.
Credentialing Timelines and Insurance Plans
Each insurance company has different requirements and timelines for credentialing. The process typically takes anywhere from 60 to 120 days, depending on the insurer and the completeness of submitted documents. Government payers may require more detailed background checks, leading to longer processing times. However, some commercial insurers offer faster electronic processing, which can expedite the credentialing process.
Consequences of Poor Credentialing Management
Inefficient credentialing management can significantly impact family practices which eventually leads too:
Delayed/Denied Payments: Errors in credentialing can cause payment delays or denials.
Lost Revenue: Non-credentialed providers may result in unreimbursed services.
Patient Dissatisfaction: Providers not listed as in-network can frustrate patients.
Compliance Risks: Failure to meet credentialing standards can lead to legal and regulatory issues.
Damaged Reputation: Poor credentialing management can damage a practice’s reputation with both insurance companies and patients.
Choosing the Best Credentialing Company
For any family company, choosing the right medical credentialing company is a very important choice. The key characteristics that all of the best credentialing companies have in common are:
Extensive Experience: A reputable credentialing partner should have a proven track record of success across multiple payer systems and provider types, especially in primary care and family medicine.
Transparency: Clear communication, real-time status updates, and detailed reporting are hallmarks of a transparent credentialing service.
Technology-Enabled Solutions: Leading companies use advanced software platforms to automate application tracking, ensure timely reminders for re-credentialing, and reduce human errors.
These features not only make the identification process easier but also help keep operations running smoothly and in line with regulations in the long term.
Credentialing Services for Providers – What to Expect
Proper credentialing is essential for healthcare providers, especially in family medicine, to ensure compliance, secure timely reimbursements, and establish credibility with insurance companies. Medical Credentialing services simplify this process by offering support at every stage.
- Initial Application and CAQH Setup
The credentialing process starts with collecting personal, educational, and professional details from the provider. Accuracy is key to avoiding delays, especially when setting up and maintaining the CAQH (Council for Affordable Quality Healthcare) profile. This universal application is used by most insurers, so keeping it up-to-date is important. Credentialing services ensure the CAQH profile reflects current licensure, insurance, and credentials.
- Re-Credentialing and Ongoing Monitoring
Credentialing doesn’t stop after approval. Most insurers require re-credentialing every two to three years, and credentialing services handle this proactively, ensuring all documentation is submitted on time. Ongoing monitoring tracks license renewals, sanctions, and status changes, ensuring compliance with payer regulations.
- How Providers Can Stay Proactive
While credentialing services manage the process, providers should stay involved by keeping documents up to date, responding quickly to requests, and informing credentialing partners of any changes. Collaboration with credentialing partners reduces administrative burdens and minimizes the risk of denials and payment delays
Concluding Words
Credentialing is essential to a successful medical practice, not just a chore. Family care requires trust and continuity, thus being certified with the correct insurance networks increases patient access and practice growth. Advantages Of Credentialing are:
- Improved Patient Access
- Increased Credibility
- Practice Growth
Why Professional Support Matters
Credentialing is easier when you work with experienced people who know the requirements set by payers and regulators. Getting help from an expert can make things easier for payers, among other things.
These experts also make sure that your business follows all the rules so that you don’t get in trouble with the law. You can save time and avoid making mishaps that cost a lot of funds by giving them paperwork and routine tasks.
Long-Term Success: Partner with us to build a strong, credentialed foundation for your practice.
Find out how our reliability and precision will help with your credentialing requirements and guarantee the continued success of your practice. Reach out to Resilient MBS LLC today for expert guidance and easy credentialing solutions.










