In medical billing, modifiers are short two-character codes added to CPT (procedure) codes. They give extra details about a service, like exceptional circumstances, and help insurance companies decide if the service should be paid for.
In podiatry, the Q7, Q8, and Q9 modifiers are especially important. They apply to routine foot care, which is usually not covered by Medicare or insurance unless a medical condition makes it necessary, for example, when a patient has a systemic disease. Using these modifiers correctly shows why the care is needed, helps avoid claim denials, and keeps providers compliant with insurance rules.
Accurate use of modifiers also helps providers get paid on time and avoid audits or penalties. That’s why understanding Q7, Q8, and Q9 is essential for both good patient care and smooth billing. Let’s dive in deeply.
Understanding Podiatry Q Modifiers
What are “Q” Modifiers in Podiatry Billing?
Q modifiers are special billing codes that show when routine foot care is medically necessary under Medicare. Podiatrists and other providers use them to prove that a patient’s foot care is related to a serious health condition.
Why They’re Needed
Medicare usually doesn’t pay for routine foot care, like trimming nails, removing calluses, or treating corns. However, if a patient has a condition such as diabetes or poor circulation, these services may be covered because they help prevent serious complications.
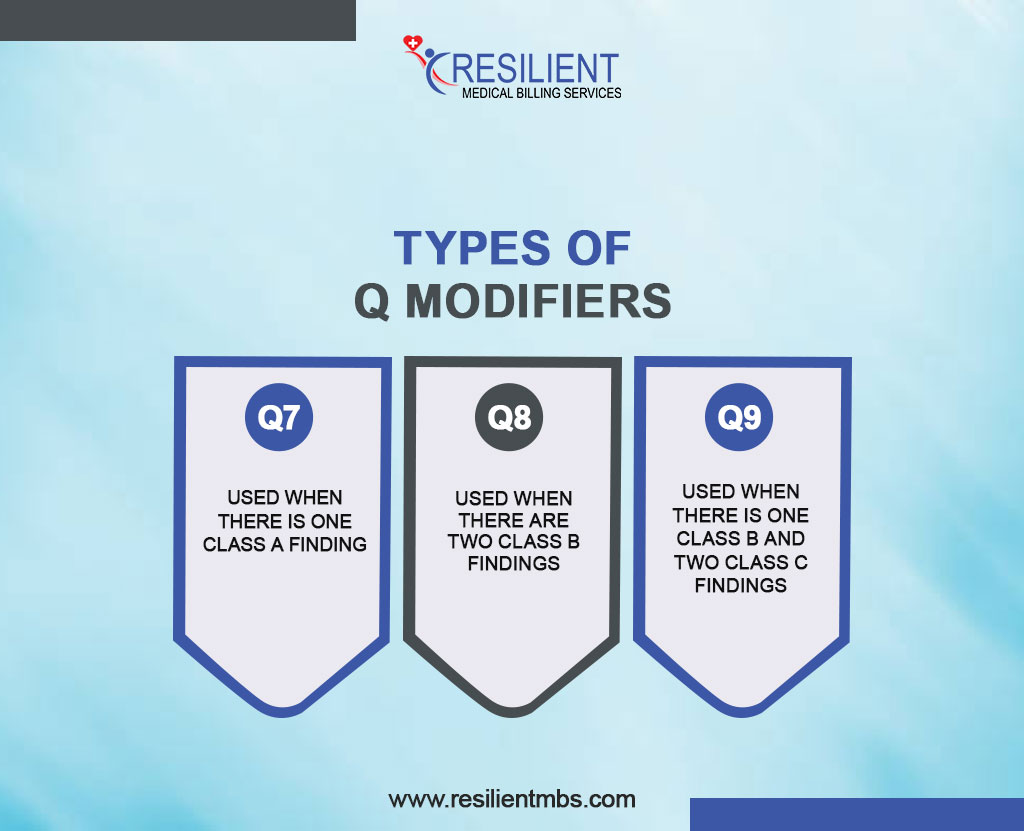
Types of Q Modifiers
Q7: Used when there is one Class A finding (for example, a non-traumatic foot amputation).
Q8: Used when there are two Class B findings (like no dorsalis pedis pulse or severe skin changes).
Q9: Used when there is one Class B and two Class C findings (such as swelling, tingling, or burning pain).
By adding these codes to claims, providers show insurance companies why the care is necessary and increase the chances of payment approval.
Coverage in Simple Terms
Routine foot care is not usually covered. But if a systemic condition—like diabetes—puts the patient at risk of infection or complications, Q modifiers help prove medical necessity. Accurate documentation and correct use of modifiers are essential for getting claims paid.
Modifier Q7
Q7 Modifier Description: One Class A Finding
The Q7 modifier is used when a patient has a serious condition called a Class A finding, which usually means part of the foot has been amputated (removed). This shows that routine foot care is medically necessary because these patients are at high risk for further problems.
What qualifies? Loss of a toe, part of the foot, or the whole foot (often from diabetes or poor circulation).
Examples:
- A diabetic patient who lost a toe and now needs nail care.
- A patient with part of the foot removed due to vascular disease who needs regular foot care.
Q8 Modifier: Two Class B Findings
The Q8 modifier is used when a patient has two Class B findings, which are health issues that affect circulation and skin health in the feet. Examples include weak or absent pulses, skin changes like thinning or thick nails, or pain from poor blood flow.
Examples:
- A diabetic patient with no detectable pulse in the foot and skin changes from poor circulation.
- A patient with delayed capillary refill and visible changes in the skin and nails.
Tip for providers: Make sure records clearly show the two Class B findings, using exam notes or test results.
Q9 Modifier: One Class B and Two Class C Findings (Most Common)
The Q9 modifier applies when a patient has one Class B finding plus two Class C findings. Class C findings are less severe but still significant, such as swelling, numbness, tingling, or burning in the feet.
Examples:
- A patient with no foot pulse (Class B) plus swelling and numbness (Class C).
- A patient with skin changes (Class B) plus burning and swelling (Class C).
- A vascular patient with poor blood flow (Class B) plus numbness and edema (Class C).
Why Modifier Q9 Is Important in Podiatry Billing
Modifier Q9 is used when a patient has a mix of foot health risks—one moderate issue (Class B) and two more minor issues (Class C). Using this code tells Medicare or insurance that the foot care is medically necessary, not just routine. Without Q9, the claim might be denied.
How Q9 Is Different from Q7 and Q8
Q7: One serious condition (Class A).
Q8: Two moderate conditions (Class B).
Q9: One moderate (Class B) + two minors (Class C).
Q9 helps cover patients who don’t fit the exact rules of Q7 or Q8 but still need essential foot care.
Correct Use of Q Modifiers in Podiatry Medical Billing
Q7, Q8, and Q9 modifiers are used in podiatry billing to show when foot care is medically necessary, not just routine. Medicare and other payers only accept these modifiers if the patient’s medical records clearly support them.
A common mistake is using the wrong modifier, such as Q8 (two Class B findings), when only one Class B finding is documented. Another error is applying a modifier without proof, like missing details about poor circulation or other qualifying conditions. To prevent denials, podiatrists should always back up modifiers with detailed notes, exam results, and patient history. Good documentation proves medical need and protects providers if claims are audited.
Impact on Reimbursement and Compliance
Using Q modifiers correctly helps podiatrists get paid on time, avoid claim denials, and stay compliant with insurance rules. Accurate coding keeps revenue flowing and reduces delays.
On the other hand, incorrect use can lead to denials, more paperwork, and even compliance risks. For example, a claim with a well-documented Q9 (one Class A and one Class B finding) is far more likely to be approved than one missing the required evidence. This shows why accuracy in modifier use is so important for both financial health and compliance.
Concluding Words
Q7, Q8, and Q9 modifiers are very important in podiatry billing because they show when foot care is medically necessary. Using them correctly, along with good documentation, helps providers follow Medicare rules, prevent claim denials, and keep their payments steady.
Need help with podiatry billing? Contact Resilient MBS today, and we’ll help you use modifiers the right way, stay compliant, and get the reimbursements you deserve.
FAQs
What are Q7, Q8, and Q9 modifiers in podiatry?
These are special billing codes used in podiatry to show that a patient has certain foot conditions. They help Medicare and insurance know when routine foot care is medically necessary.
What does the Q7 modifier mean?
The Q7 modifier is used when the patient has one serious foot problem (Class A finding), like a foot amputation that wasn’t caused by an injury.
When is the Q8 modifier used?
The Q8 modifier is added when the patient has two moderate foot problems (Class B findings), such as poor blood flow or other signs of circulation issues.
What does the Q9 modifier show?
The Q9 modifier is used when the patient has one Class B finding and two Class C findings. This combination proves that routine foot care is needed and should be covered.
Why do Q modifiers matter in podiatry billing?
Using Q7, Q8, and Q9 modifiers correctly helps podiatrists get paid for their work, prevents claim denials, and makes sure patients get the care they need without delays.










