The healthcare revenue landscape in 2026 is evolving faster than ever. With new payer regulations, tighter reimbursement models, and advanced technologies reshaping workflows, optimizing medical billing is no longer optional; it’s vital for survival.
Optimizing medical billing means more than faster claim submissions. It’s about ensuring accuracy, compliance, and financial consistency at every step. When healthcare organizations strengthen their billing workflows, they minimize claim denials, accelerate reimbursements, and safeguard long-term revenue health.
This guide shares ten proven strategies to optimize medical billing in 2026; practical, evidence-based steps every healthcare organization can apply to enhance efficiency, accuracy, and profitability.
Understanding Medical Billing Optimization
Medical billing optimization is the process of refining and improving every aspect of the billing cycle to ensure claims are submitted, tracked, and reimbursed with precision and speed. It blends automation, data analytics, and staff expertise to eliminate inefficiencies and maximize reimbursements.
With 2026 bringing advanced AI tools, stricter payer policies, and growing administrative demands, healthcare practices must leverage smart billing systems to stay compliant and competitive.
Optimized billing systems:
- Prevent revenue leakage and claim denials.
- Strengthen compliance with payer and federal guidelines.
- Improve patient satisfaction through accurate billing and transparency.
Strategy 1: Automate Repetitive Billing Tasks
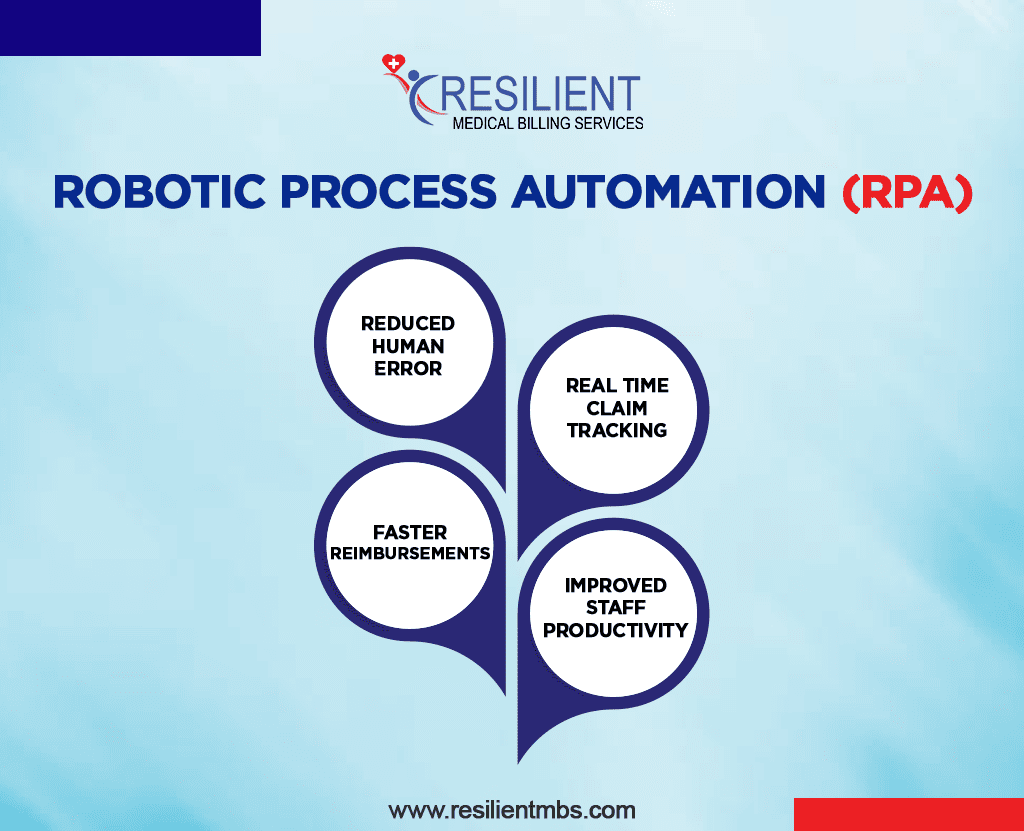
Automation has become the cornerstone of modern medical billing. By automating tasks such as claim submissions, payment posting, and denial follow-ups, providers reduce manual errors and processing delays.
AI-driven billing systems and Robotic Process Automation (RPA) now streamline claim handling and identify potential issues in real time, ensuring a faster and cleaner billing process.
Benefits:
- Reduced human error
- Real-time claim tracking
- Faster reimbursements
- Improved staff productivity
Pro Tip: Integrate your EHR system with your billing platform for real-time data sharing and workflow automation, a key step in medical billing optimization.
Strategy 2: Ensure Accurate Patient Data Collection
Accurate patient information is the foundation of a successful billing cycle. Even minor errors, an incorrect policy number or outdated address, can result in claim denials or delays.
Best practices for accuracy:
- Verify insurance eligibility before every visit.
- Use digital intake forms to reduce typing errors.
- Train front-desk teams to validate every data point.
- Sync EHR and billing software for real-time updates.
Accurate data ensures first-pass claim success and strengthens patient trust, both crucial for optimizing medical billing in 2026.
Strategy 3: Conduct Regular Coding and Compliance Audits
Medical coding errors can drain thousands in lost revenue. Regular ICD-10 and CPT coding audits are essential to maintain compliance and avoid payer penalties.
Audits help detect errors early, assess staff performance, and ensure complete documentation. In 2026, AI-based audit tools will make it easier to flag inaccuracies and prevent repeat mistakes.
Action Steps:
- Schedule quarterly coding reviews.
- Train staff on recent code updates.
- Maintain detailed documentation for every billed service.
- Partner with certified coders for expert oversight.
This not only supports compliance but also builds credibility and financial integrity.
Strategy 4: Invest in Staff Training and Certification
A knowledgeable billing and coding team is one of your strongest assets. Ongoing education keeps staff aligned with payer policy changes and coding updates, reducing claim denials and compliance risks.
Certified professionals also enhance your organization’s credibility and EEAT reputation by ensuring ethical and accurate billing.
Investing in your team = investing in your revenue.
Encourage certifications such as CPC (Certified Professional Coder) or CPB (Certified Professional Biller) for higher efficiency and compliance assurance.
Strategy 5: Leverage Data Analytics for Smarter Decisions
Data-driven billing is the future. Through analytics dashboards, healthcare organizations can identify revenue bottlenecks, monitor KPIs, and forecast cash flow accurately.
Key metrics to track:
- Clean Claim Rate (CCR)
- Denial Rate
- Days in Accounts Receivable (A/R)
- Net Collection Rate
Analytics help you pinpoint trends, uncover claim errors, and measure staff performance, enabling continuous improvement in medical billing practices.
Strategy 6: Strengthen Communication Between Billing and Clinical Teams
Poor communication between billing and clinical staff often leads to coding errors and delayed claims. Regular collaboration ensures that provider notes are complete and documentation aligns with billing requirements.
How to strengthen collaboration:
- Hold monthly review meetings.
- Use shared digital workspaces or billing dashboards.
- Encourage open feedback between teams.
This alignment enhances accuracy, compliance, and ultimately, patient care, reinforcing the trust factor central to EEAT.
Strategy 7: Use Advanced Medical Billing Software
Modern billing software is a game-changer. Look for systems that offer:
- Real-time eligibility checks
- Built-in compliance alerts
- Predictive analytics
- Automated denial management
In 2026, AI-powered billing software not only automates workflows but also provides insights that help practices forecast revenue trends and optimize reimbursement cycles.
Strategy 8: Outsource to Professional Medical Billing Companies
Partnering with a professional medical billing company like Resilient MBS can drastically improve efficiency, reduce costs, and ensure full compliance.
Outsourcing allows providers to focus on patient care while experts handle billing complexities, from coding and claim submission to denial resolution.
Benefits of outsourcing include:
- Access to certified billing experts
- Faster claim turnaround
- Reduced administrative workload
- Scalable solutions for busy practices
Explore how Resilient MBS helps healthcare providers optimize medical billing through automation, compliance, and analytics-driven solutions.
Strategy 9: Strengthen Denial Management Processes
Denial management directly impacts your bottom line. Every denied claim represents lost or delayed revenue. The key is to identify, analyze, and resolve denials quickly.
Effective denial management steps:
- Track all denials in a centralized system.
- Identify root causes and recurring payer issues.
- Develop a standardized denial appeal workflow.
By monitoring trends and training staff to prevent common errors, practices can achieve up to a 30% reduction in claim denials, a core goal of efficient medical billing optimization.
Strategy 10: Monitor KPIs and Continuously Improve Processes
Optimization is an ongoing process. Tracking Key Performance Indicators (KPIs) ensures your billing system evolves with payer and regulatory changes.
Regularly assess:
- Claim approval rates
- Days to payment
- Denial trends
- Compliance audit results
A data-driven review cycle allows you to refine workflows, eliminate bottlenecks, and maintain long-term financial health.
Common Challenges in Medical Billing Optimization: Proven Tips and Tricks
Even top-performing practices face billing hurdles.
Common issues include:
- Delayed documentation
- Payer communication gaps
- Software incompatibilities
Easy Steps to Efficient Medical Billing:
- Automate repetitive claim tasks.
- Upgrade to AI-enabled billing software.
- Conduct monthly process audits.
- Maintain staff certification and compliance training.
A proactive approach not only prevents revenue leakage but also ensures steady growth and regulatory compliance.
Closing Words
Optimizing medical billing in 2026 is not just about faster payments; it’s about building a resilient, transparent, and compliant financial ecosystem.
By adopting automation, investing in training, analyzing performance metrics, and outsourcing strategically, healthcare providers can maximize revenue and minimize stress.
For expert support and customized billing optimization solutions, contact Resilient MBS, your trusted partner in accurate, compliant, and profitable medical billing.
FAQs
What does it mean to optimize medical billing?
It means improving billing accuracy, minimizing claim denials, and using automation and analytics to accelerate reimbursements.
Why is medical billing optimization crucial in 2026?
Evolving payer rules and technology updates make optimization essential for faster payments and better compliance.
What are some best practices in medical billing?
Regular audits, staff certification, automation, denial tracking, and advanced analytics.
How does automation improve medical billing?
Automation minimizes manual errors, accelerates claim processing, and improves cash flow consistency.
Is outsourcing medical billing a good option?
Yes. Partnering with experts like Resilient MBS ensures accuracy, compliance, and optimized revenue cycle performance.










