For uniformed service members, retirees, and their families in the USA, TRICARE is essential to providing comprehensive health services. TRICARE, managed by the Defense Health Agency, covers health, special programs, medicines, and dental plans.
Military insurance is about helping the US military and boosting healthcare providers’ patient bases. Providers show their dedication to military service and quality care.
Tricare Credentialing is essential for providers to meet TRICARE criteria. This checks a provider’s education, training, experience, and licensure. Providers must be qualified and experienced to provide great treatment to TRICARE beneficiaries.
This credentialing is more than a checkbox for physicians; it shows trust and credibility. It shows patients and insurance networks, including TRICARE, that providers meet high criteria and are dedicated to providing the finest care to veterans.
What is TRICARE Credentialing?
It is the process through which active duty personnel, retirees, and their family members are issued authorization to receive services from specific healthcare practitioners.
This includes reviewing the provider’s education, training, background, competence, and whether he or she is legally allowed to provide services.
The major reason for TRICARE credentialing is the guarantee of the fact that all providers involved in the TRICARE network are qualified and capable of providing the recipients with high-quality treatment that would protect their health and contribute to the well-being of the military personnel and their families.
Steps for TRICARE Credentialing
Sending an Application
Fill out an application form and send it to TRICARE with the necessary papers for review.
Checking Your Credentials
TRICARE checks your credentials, such as your schooling, training, licenses, and certifications.
Approval Process
Once your identity has been confirmed, TRICARE will look over your application and grant your credentials if you meet their standards.
Importance for Military Family Providers
Providers need Tricare accreditation for several reasons. First, it provides access to TRICARE patients military personnel, retirees, and their families.
Second, TRICARE-authorized providers are dedicated to providing high-quality treatment to a distinct and deserving population, boosting professional reputation.
Third, joining Tricare can enhance patient referrals and income since many military families prefer Tricare-covered providers. Finally, TRICARE provides network providers training, policy updates, and claims and invoicing assistance.
TRICARE Credentialing for Behavioral Health Providers
This type of credentialing covers uniformed service members, retirees, and their families worldwide, and requires mental health providers to be credentialed. These regulations ensure providers meet care and competency standards.
Some key considerations for behavioral health credentialing with TRICARE include:
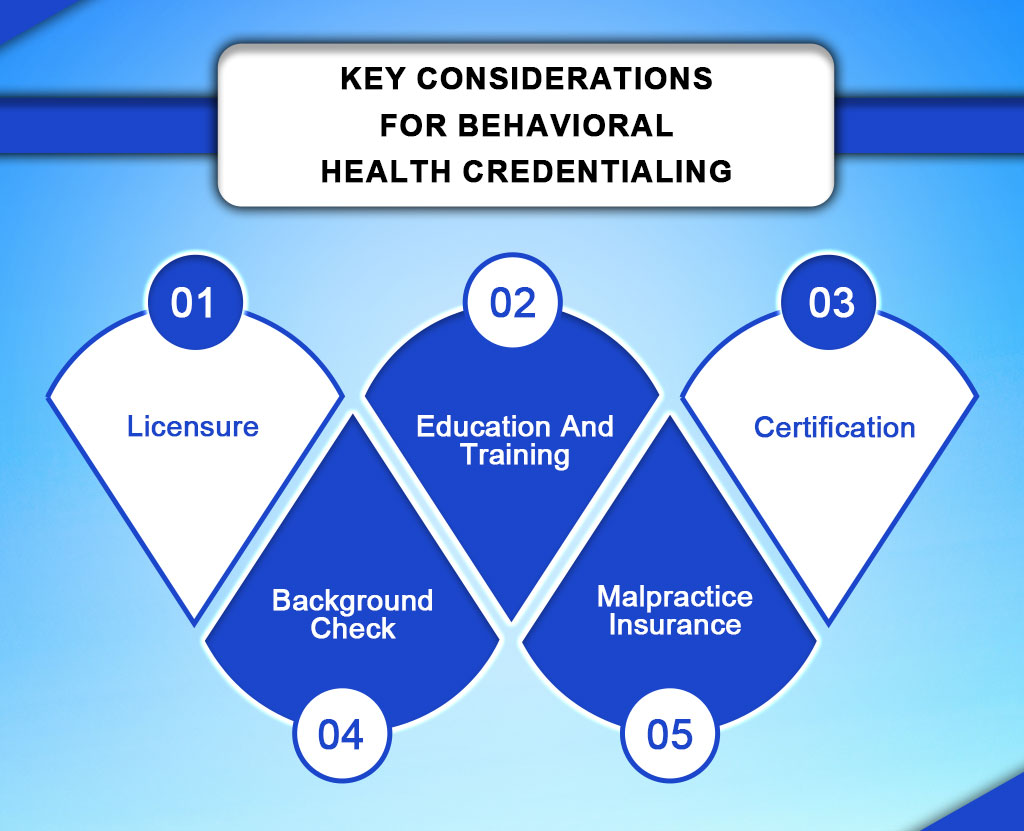
Licensure
Providers must also be current and clear to practice independent practice in their state or country. Containing the license, this agreement must correspond to the provider’s specialty and scope of practice.
Education and Training
It requires that BH professionals have appropriately completed a graduate or postgraduate program in specialty areas of practice, e.g., psychology, SW, or counseling. They should also possess proven course and vocational aptitude in handling mental health disorders.
Certification
It is important to recognize that some types of behavioral health providers, depending on their specific scope of practice, may require other forms of certification and/or licensure, which may include board certification in psychiatry or as an addiction counselor.
Background Check
Malpractice Insurance
Every health care provider is required by law to obtain professional liability insurance to cater for the cost when found legally liable to a patient for an act in the course of his practice.
Difference Between Paneling and Credentialing
Paneling entails applying, meeting standards, and signing a contract to join a healthcare network like TRICARE. This lets providers accept network patients, increasing their patient base and revenue.
Credentialing checks a provider’s qualifications, expertise, and background to fulfill network or payer criteria. Validating licenses, education, training, and other credentials shows competence
and compliance with legislation.
Practitioners need panels to increase patient access revenue and credentialing to ensure quality care, regulatory compliance, and insurance coverage.
Paneling and credentialing affect patient attractiveness, reimbursement fee negotiation, and network access for providers. They also ensure qualified providers accept insurance, improving patient access to care.
Contact Us Today!
To become a part of the TRICARE networks, paneling, and Tricare credentialing must be formed by the healthcare providers. Credentialing is crucial since it verifies the provider’s credentials and quality to produce qualitative care while paneling enables an increased number of patients. Patient care and service considerations require that providers seek TRICARE accreditation to enhance the system.
There is no need to wait let’s begin to credential TRICARE healthcare providers today! Please seek our assistance at Resilient MBS; we are ever willing to assist you in any way that we can. As ONE, we can enhance the quality of care given to TRICARE beneficiaries.