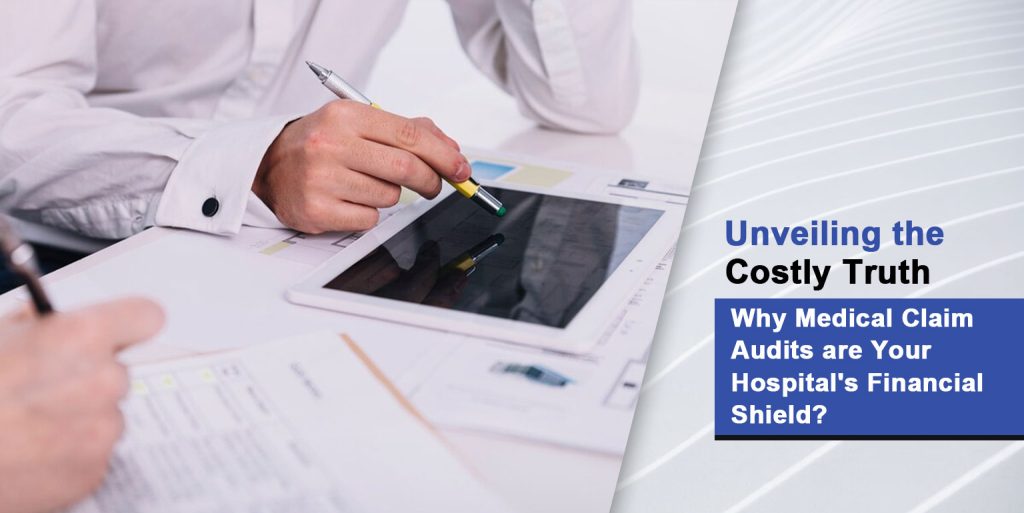
It reports every year that a huge amount of money is spent on healthcare areas that make medical claim audits a mandatory burden.
Simply a small mistake with billing may induce all to be knocked down by the domino stone effect so that it will encompass not only the profit but also the patient’s health.
Medical claim audit avoids this by scrupulously reviewing medical claims to detect if they are accurate and in line with regulations.
A report published last year discovered that in just one year Medicaid had distributed $36 billion in mistaken claims.
Claims audits have a role in a corrective process that brings the discrepancies to the fore, ensuring that patient interests are protected while healthcare providers’ reputations are maintained.
But here’s a bigger blow – nearly 80% of medical bills have errors. Surprised? Such a lot is at stake and that’s why it is necessary that medical claim audits be frequent in your hospital to protect its financial strength.
That’s it! Now, we will actually look into the key facts of medical claim audits in this article.
What is the Main function of the Claim Audits?
The purpose of a Medical Claim audit is to check the providers’ billings for accurate information prior to submitting the claims to the insurance companies and government programs’ program to make sure that everything is correct and is in compliance with the regulations.
Objectives Of Medical Claims Audit
The primary objectives of the medical claim audit are to maintain the legality of the billing practices and the correct remuneration of the medical claims.
Ensuring Compliance with Regulations
Healthcare providers must follow government laws and processes like ICD-10 and CPT codes to ensure proper operations. This is essential to avoid money loss by discovering and fixing errors, fairly compensating providers, and accurately charging patients.
Audits also help prevent fraud and abuse by identifying and eliminating improper billing practices including charging for services not performed or using inaccurate codes.
Regular audits support honest billing, fostering patient trust and healthcare system integrity. The viability and integrity of healthcare operations depend on medical claim audits to ensure compliance, prevent fraud, and maintain billing honesty.
Finding Billing Errors and Overcharges
Medical billing errors must be found to ensure accuracy and fairness. Audits reveal flaws and overcharging that may have gone undetected.
The American Medical Association reports that 10% of claims are paid wrongly due to minor errors, which might cause financial problems. Audits discover and fix these errors, saving healthcare providers money and ensuring they are paid fairly, benefiting both providers and patients.
Fraud Prevention and Billing Integrity
Audits prevent healthcare billing fraud and misuse. They detect and stop illicit billing activities like charging for services not provided or inflating payments using inaccurate codes.
Regular audits encourage healthcare professionals to bill honestly, which builds patient trust and protects the healthcare system.
Medical claim audits ensure accuracy, billing honesty, law compliance, and fraud prevention, strengthening and ethically practicing healthcare professionals.
Benefits of a Medical Claim Audit
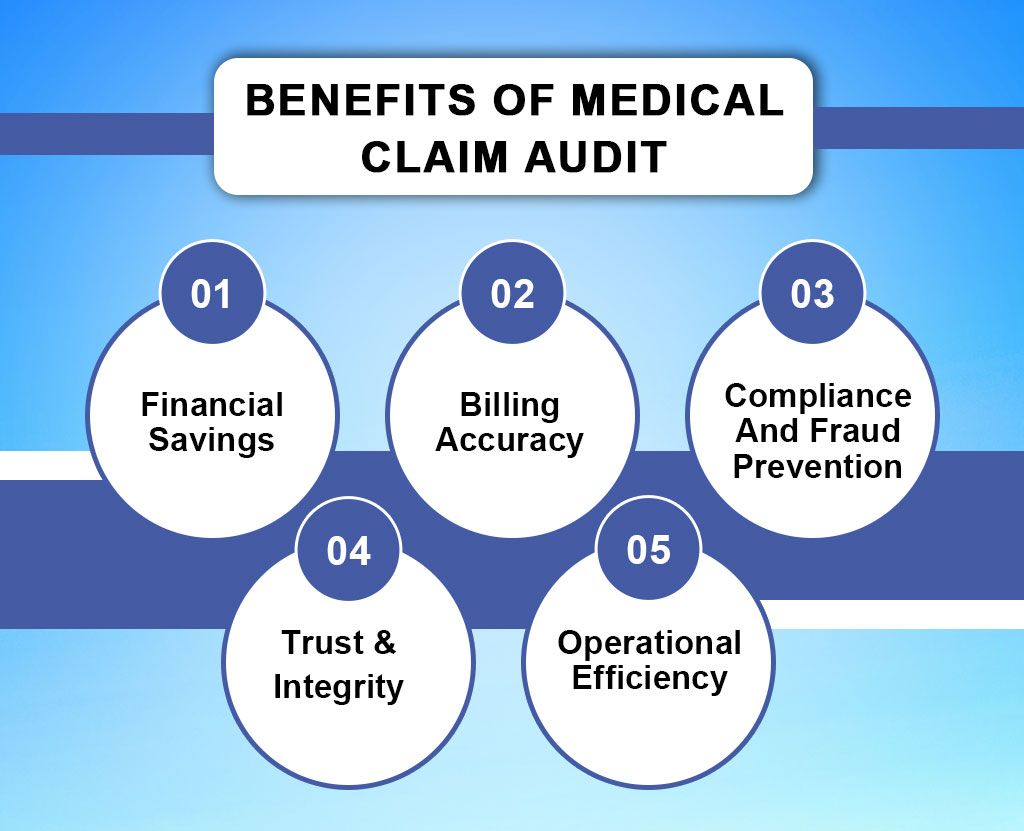
Financial Savings
Acuity of audits on medical claims can help medical providers not to reach up to 5% of their revenues through miscalculation.
Through the discovery and correction of errors and overcharging, audits minimize the chance of providers to lose money, thus ensuring that they are fairly paid for their services.
Audits have reduced Medicare fee-for-service inappropriate payments from 9.5% in 2015 to 6.27% in 2019, lowering financial losses due to billing errors, according to a CMS report.
Billing Accuracy
Accountability is guided by audits by reveal overcharging that has otherwise been undetected. This, of course, makes it possible to make sure that patients do not pay more than they should and that providers for the services allotted are reimbursed.
Compliance and Fraud Prevention
Audits are very important since they help to enforce the laws and to prevent fraud. They allow detecting and putting a stop to instances of misbilling or billing through wrong codes. Aside from this, they also prevent correct charging for services not delivered or incorrect coding and billing.
The American Association of Professional Coders (AAPC) found that audits can discover billing errors and fraud, reducing claim denials by 5-10% and increasing healthcare provider income by 2-5%.
Trust and Integrity
Routine review of medical companies ensures that they bill in honor, therefore the integrity of the healthcare system is upheld. This brings the trust of patients to the entire healthcare system.
Operational Efficiency
Through accurate billing and adherence to the guidelines, audits help to enhance the overall efficiency and sustainability of healthcare practices. They prevent medical providers from suffering from issues with the billing method or any other fraud; hence, they can concentrate on caring for their patients better.
Audits can improve income by 1-3% and decrease denials by 4-7%, according to the Healthcare Financial Management Association (HFMA).
How Medical Billing Audits are Conducted
The Medical Claims audit process is thoroughly arranged to evaluate the claims for authenticity, accuracy, completeness, and compliance with medical policies.
Medical claim audits are carried out through a methodical approach to verify the billing accuracy and conformance to the regulations. This process commonly starts off with both the processing of billing data, inclusive of patient files, treatment records, and billing codes.
Therefore, the software with specific features and tools are then run to scrutinize this data which is afterwards compared against ICD-10 codes and the CPT manual. Certified medical coders and auditors have a vital part in this process, they are the ones who check the data and find any mistakes or discrepancies.
Services Of Medical Claim Auditing
On the other hand, medical claim auditing services provide accurate financial support to patients who have medical benefits through insurance companies.
Medical billing audit firms provide a basket of services aimed at the verification of accurate billing along with compliance with regulations. These services include comprehensive audits, which is a thorough investigation of all billing data to detect errors and inconsistencies.
Alongside verification checks of code, review of them is another common practice for checking that the right code is being used for invoicing purposes. Further, independent inspections of the billing records may be made to determine if the billing policies conform to regulatory requirements.
Claim auditing services outsourcing to medical billing audit companies is a way to get a lot of advantages for healthcare providers.
Outsourcing helps providers of healthcare to focus on the core functions, eg. patient care. However, the autistic functions should be left to the experts, such as data analytics. Furthermore, outsourcing can reduce the cost of healthcare as it is no longer necessary for healthcare providers to use specialized software and train their staff.
Enhance Your Auditing Skills
Seek Resilient’s Certified Professional Medical Auditor or Certified Professional Compliance Officer credentials to demonstrate your medical chart auditing expertise and advance your career.
Try a free sample and consultation at Resilient Medical Billing to learn how it simplifies medical record retrieval.