When it comes to healthcare, accuracy in medical billing isn’t just important, it’s critical. It keeps the financial wheels turning, ensures compliance with healthcare laws, and builds trust among providers, payers, and patients alike. But let’s face it, billing isn’t always straightforward. From choosing the right codes to filing clean claims, the process is full of complexities that leave plenty of room for error.
One of the most damaging errors is medical double billing. Whether unintentional or due to system flaws, medical double billing can result in claim denials, financial losses, or even legal consequences.
As healthcare regulations tighten and oversight intensifies, providers are feeling the pressure. Duplicate billing and other compliance missteps don’t just hurt your bottom line — they put your reputation at risk.
About Double Billing in Medical Billing
Double billing in medical billing refers to the submission of more than one claim for the same service, procedure, or patient encounter. This can occur when a healthcare provider or facility bills multiple times for a single service, either to the same insurer or to different insurers. In some cases, this may happen inadvertently due to administrative errors, while in others, it may be a deliberate act of fraud.
Common Causes of Double Billing
Double billing is a major issue in healthcare, causing financial discrepancies, compliance problems, and damaging provider-patient trust.
Recognizing its common causes can help improve billing accuracy and prevent costly errors.
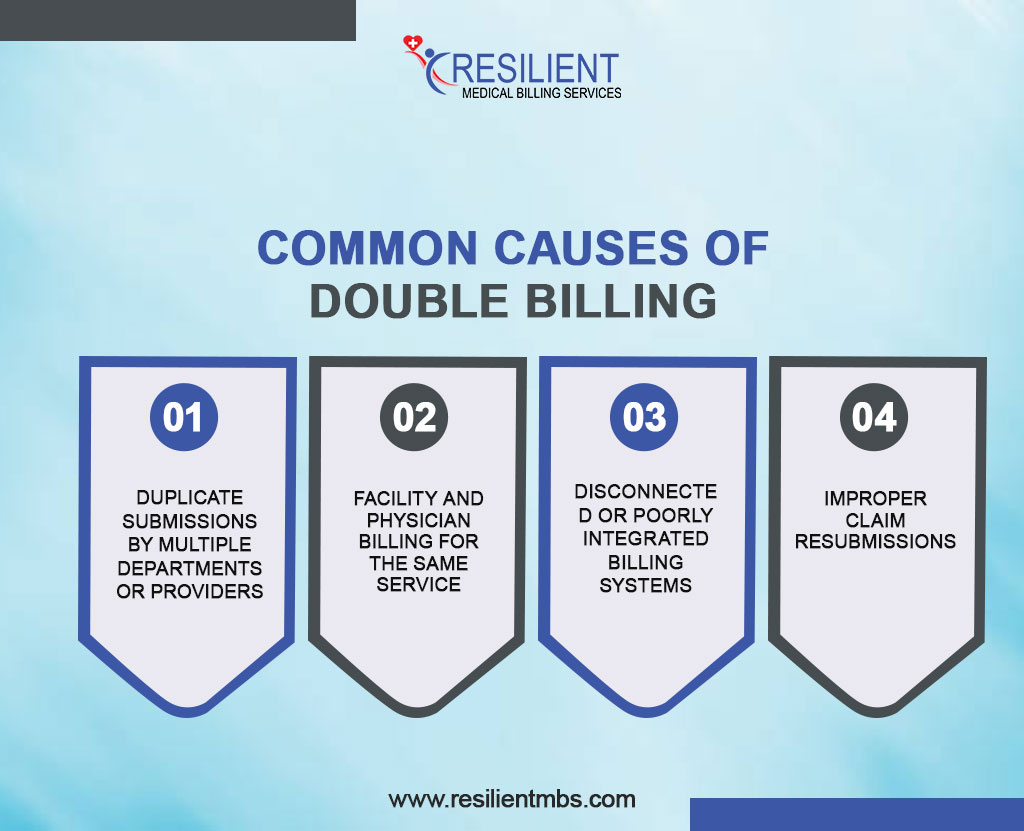
- Duplicate Submissions by Multiple Departments or Providers
Double billing often occurs when different departments or providers submit claims for the same service due to poor internal communication or lack of centralized billing oversight.
- Facility and Physician Billing for the Same Service
In hospitals or clinics, both the facility and physician may bill separately for the same procedure without coordination, leading to unintentional duplicate charges.
- Disconnected or Poorly Integrated Billing Systems
Using multiple billing platforms or EHRs that don’t sync can result in duplicate claims due to inconsistent data or system errors.
- Improper Claim Resubmissions
Resubmitting denied claims without addressing the original denial or tracking previous submissions can lead to duplicate billing. Strong denial management practices are key.
Is Double Billing Illegal?
Double billing goes beyond a simple billing mistake; particularly with government programs like Medicare and Medicaid, it can have major legal repercussions.
Submitting duplicate claims, whether intentional or accidental, may be treated as double billing insurance fraud. Insurers can deny claims, demand repayments, impose fines, or initiate legal action.
Under federal law, Medicare double billing violates the False Claims Act and can trigger audits, penalties, and prosecution. The Office of Inspector General (OIG) actively monitors and investigates such cases using data analytics and audits.
Can Double Billing Occur Unintentionally?
Yes, double billing can occur unintentionally, especially in complex healthcare settings with multiple providers and disconnected systems. Without criminal charges, regulators may give warnings or request repairs, but providers must be cautious through audits and internal controls.
How to Prevent and Resolve Double Billing Issues
If you charge twice for the same service, it may damage your practice’s image, cause payments to be late, and lead to audits. Use these key techniques to stop it:
- Implement Billing Controls: Use clear procedures and regular audits to catch errors early. Assign roles and enforce checks and balances.
- Train Staff: Educate billing teams on coding, compliance, and documentation to avoid duplicate claims.
- Use Smart Software: Invest in billing systems that flag duplicate entries before submission.
- Hire Experts: Work with billing specialists or consultants for audits, compliance, and process improvements.
- Act Fast if It Happens: Identify the issue, inform payers or patients, correct the claim or refund, and update internal processes.
Closing Thoughts!
Double billing in medical billing refers to the act of charging twice for the same service, either intentionally or due to oversight. While it can lead to payment delays, denied claims, or even legal implications, it’s a preventable problem when practices put the right systems in place.
Healthcare is complex and requires diligence. Training staff, using the correct tools, and evaluating systems routinely can help your medical facility avoid costly billing issues and focus on quality care.
Check your financial processes often to make sure they are correct and follow the rules. For billing checks, compliance reviews, and double billing, you need to talk to a professional.
Resilient MBS offers practice-specific solutions, audits of bills, and checks for compliance. Our experts fix payment issues and make sure that businesses follow the rules. Visit our website or contact us to see how we can simplify your billing and prevent costly mistakes.










