Healthcare substance abuse billing helps people with an addiction recover. In 2020, Over 21 million Americans aged 12 and older needed substance abuse treatment (SAMHSA, 2021). This shocking number shows how vital inpatient care centers are. However, these places often have big problems with money. They must get paid correctly and on time to keep offering essential services.
Accurate billing is essential for these places to stay in business and give patients the best medical and therapeutic care while they heal. By ensuring they handle their money well, these places can focus on what they do best: helping people get better.
Understanding Substance Abuse Billing
The process of financial dealings and submitting charges for addiction to drugs or alcohol, as well as the help and rehabilitation processes, is known as substance abuse billing. This area involves complex billing codes for treating addiction alongside intricate insurance policies.
Process Involved in Substance Abuse Billing And Treatment
Billing for substance abuse treatment encompasses several essential components:
- Insurance Verification
- Proper Coding(such as CPT and HCPCS codes)
- Documentation
- Claim Submission
- Billing Compliance
Specific Substance Abuse Billing Challenges
More Denied Claims
Drug rehab centers are having problems recouping claims as more are refused. Increased reimbursement denials are hurting rehab clinics’ financial flow. Substance abuse and mental health patients cannot be treated together. They cannot bill similarly either. Healthcare providers must accurately bill patients.
Greater Patient Accountability
Most insurers consider drug use optional. Patients are not accountable for mental illness. Mental health patients get reimbursed more than addiction patients. Drug addicts must pay for rehab.
Lack of Billing Expertise
Medical billing is complicated, and substance abuse billing is even more so. Treatment facilities and mental health organizations that manage billing and collections in-house are likely losing money. Even with years of substance misuse treatment facility billing experience, reimbursements may not improve. Drug and alcohol rehabs throw away 20-30% of their revenue.
ICD-10 Codes
ICD-10 success demands knowledge of dozens of behavioral health and substance addiction billing codes. ICD-10’s hundreds of behavioral healthcare billing codes, including substance abuse therapy, can be intimidating. Medically supervised withdrawal and child substance abuse clinics can seem unending.
Inpatient Rehab Billing
Inpatient rehabilitation for substance abuse is one of the crucial elements of substance abuse treatment programs because, in this setting, the patient needs immediate and intensive care and support. It is crucial for healthcare providers and centers that are engaged in the provision of specialty services to have adequate knowledge of the billing requirements as well as requirements of the law.
CMS Inpatient Rehab Billing Guidelines
The Centers for Medicare and Medicaid Services (CMS) establishes stringent guidelines for billing inpatient rehabilitation services. These guidelines ensure quality care standards and proper financial practices within healthcare facilities.
Specific Rules for Billing Inpatient Rehab Services
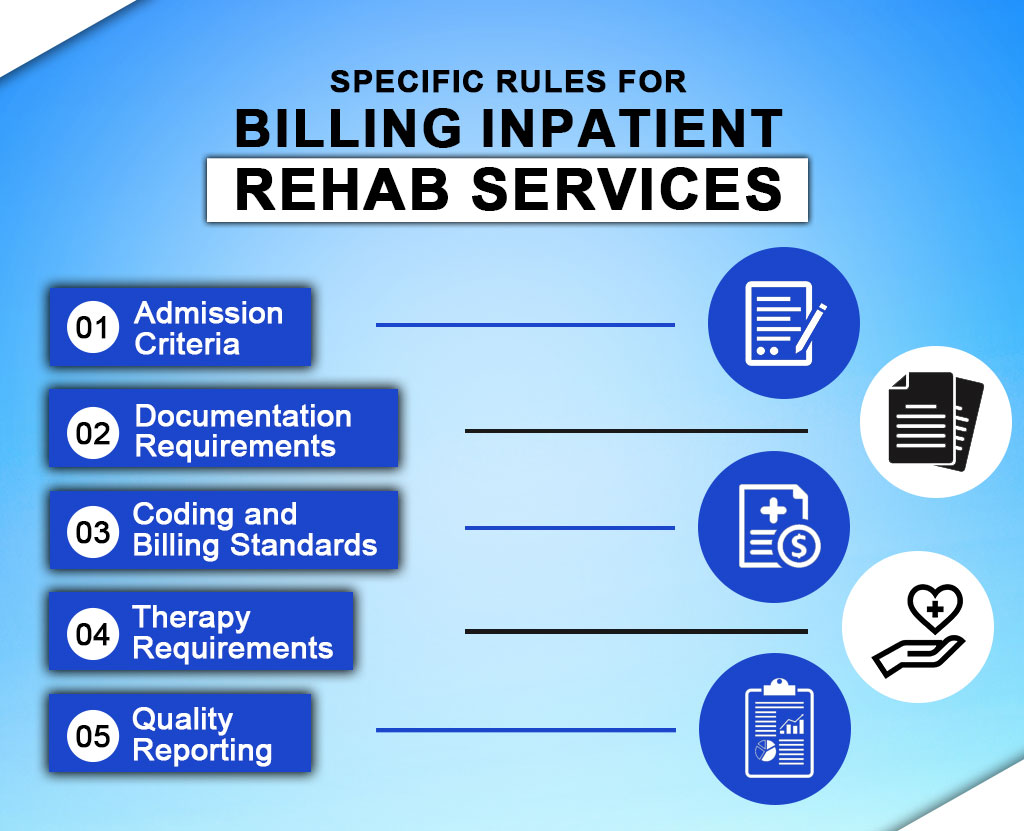
Admission Criteria
Typically, CMS has set specific guidelines for admitting patients into inpatient rehabilitation facilities IRFs. This shows that these extraordinary facilities offer intense rehabilitative services that cannot be provided in a less intense unit.
Documentation Requirements
Record keeping of the assessments made on the patient, the plan formulated for the patient, the notes taken throughout the treatment, and the summary report or discharge summary is critical. This is in contrast to CMS, which calls for rich documentation about the medical necessity of inpatient rehabilitation services.
Coding and Billing Standards
IRFs must follow CMS coding and billing rules and regulations for diagnosis ICD-10 and procedure HCPCS. This is important because coding facilitates invoicing the correct charges to reimburse the offered services.
Therapy Requirements
CMS guidelines state the expectations of the intensity of the therapy and one of the conditions is 3 hours/day, five days/week. It entails professional-recommended physical therapy, occupational therapy, and or speech-language therapy.
Quality Reporting
Substance Abuse Therapy Billing Can Earn Millions Without Clients Knowing
The billing for Substance abuse is more complicated than it looks. This is when the issue becomes severe and reduces the provider’s cash flow. This is because it takes more work for the provider to recover insurance money from the patient after receiving the check.
The buyer has cashed it numerous times and may have squandered it. Many providers’ cash flow has suffered since distributing cheques directly to patients. West Palm Beach, Miami, Florida drug rehabilitation should require the cover to sign and swear to an AOB.
The law that applies in this case is Florida – Statute 627.638, which says:
Section (1) says that an insurance contract “may” let the insurance company send the payment for a substance abuse bill straight to the service provider if the policy says so and the insured person signs off on the benefits.
Part (2) of this rule clarifies that the insured person, not just the patient, must pay the provider once they have signed and attested to the AOB.
Conclusion
It is necessary to bill appropriately for substance abuse therapy to receive effective therapy for the clients. Timely billing assists treatment centers in generating income and running profitably. Substance abuse billing requires practitioners to update themselves frequently with the set regulations and standards.
Resilient MBS provides expert therapist billing suggestions in all the above areas. Contact us today. Our niche areas of focus are Revenue Cycle and Regulatory Compliance.
If billing is a problem, Contact Resilient MBS to simplify substance abuse billing and concentrate on the patient.